-
PDF
- Split View
-
Views
-
Cite
Cite
Alaa Zayed, Enas Samara, Abdalhakim Shubietah, Ahmad Awwad, Zaid Zakaria, Rawan Daraghma, Mohammed Hajhamad, Delayed presentation of splenic laceration in a postpartum patient: a case of wandering spleen, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae499, https://doi.org/10.1093/jscr/rjae499
Close - Share Icon Share
Abstract
Wandering spleen (WS) is a rare condition where the spleen is abnormally mobile due to lax or poorly developed ligaments, leading to complications like torsion and laceration after trauma. We describe a case of a 31-year-old postpartum female who presented with severe abdominal pain following blunt trauma. Diagnostics showed an enlarged, ectopic spleen, and significant hematoma. Surgical exploration revealed a 10-cm splenic laceration, necessitating a splenectomy due to extensive blood loss and organ damage. This case highlights the challenges of diagnosing WS, particularly in postpartum patients with increased ligamentous laxity, emphasizing the need for vigilant monitoring and potentially preventive surgical measures to manage this complex condition effectively.
Introduction
Wandering spleen is a rare medical condition characterized by abnormal mobility of the spleen due to the laxity or underdevelopment of its supporting ligaments. As a result, the spleen can migrate from its typical anatomical location in the left upper quadrant of the abdomen [1]. Wandering spleen is a rare clinical occurrence with fewer than 500 cases reported and an incidence of less than 0.2% [2].
Diagnosing a wandering spleen can be challenging due to the variety of symptoms it may present, which include an asymptomatic palpable mobile mass, abdominal pain associated with a mass, or acute abdomen [3]. The unusual anatomical position of a wandering spleen leads to the vascular pedicle typically stretching and moving freely, increasing the risk of torsion and resulting in splenic infarction [4]. Imaging modalities such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) are typically used for diagnosis. These modalities aid in both confirming the diagnosis and assessing potential complications [5].
In cases where a wandering spleen becomes lacerated, the diagnosis is often delayed due to the rarity of the condition and the nonspecific nature of the symptoms. Laceration of a wandering spleen can occur following trauma and may not be immediately evident, complicating the clinical picture and leading to significant morbidity if not identified and managed promptly [6].
In this case report, we describe a 31-year-old female who presented with severe abdominal pain following a history of blunt abdominal trauma postpartum. On admission, the patient exhibited hypotension, tachycardia, and marked diffuse abdominal tenderness. Subsequent imaging and surgical exploration confirmed a diagnosis of a wandering spleen with a significant splenic laceration. This case underscores the diagnostic challenges posed by the rare occurrence of a wandering spleen, especially when complicated by trauma.
Case presentation
A 31-year-old female with an unremarkable past medical and surgical history presented to the emergency department complaining of severe abdominal pain. She reported that two weeks prior to this incident, she had undergone her second normal vaginal delivery without any complications. Additionally, she experienced blunt abdominal trauma from falling onto a hard floor ten days earlier. Ten days following the trauma, she began to experience dull, aching, diffuse abdominal pain, although she reported no fever, nausea, vomiting, urinary symptoms, or vaginal discharge.
Upon admission to our hospital, the patient’s physical examination revealed hypotension (87/52 mmHg) and tachycardia (150 bpm), along with marked diffuse abdominal tenderness and guarding. Laboratory investigations indicated a hemoglobin level of 7.1 g/dl, a white blood cell count of 14.5 × 103 μl, and a platelet count of 202 × 103 μl. An abdominal CT scan without contrast showed an enlarged ectopic spleen measuring 18 cm in the right abdominal area, a distended stomach, a moderate volume of hemoperitoneum, and significant intra-abdominal fluid accumulation. CT findings are shown in Figs 1–3. Based on these findings, the patient was immediately transferred to the operating room.

Noncontrast coronal CT scan of the abdominopelvic area showing the spleen located in the right upper abdominal area.
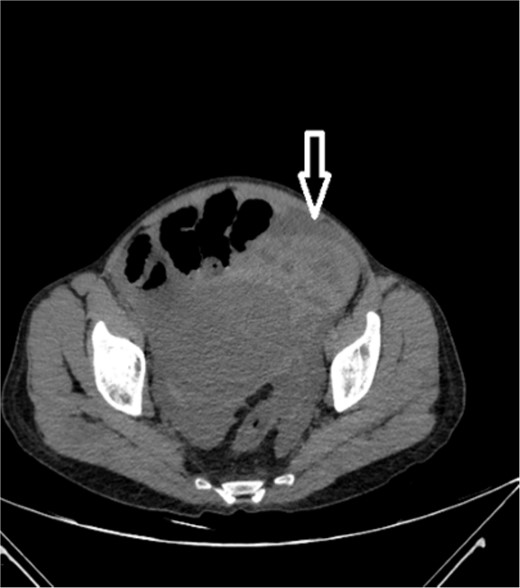
Noncontrast axial CT scan of the abdominopelvic area showing a left-sided pelvic hematoma.
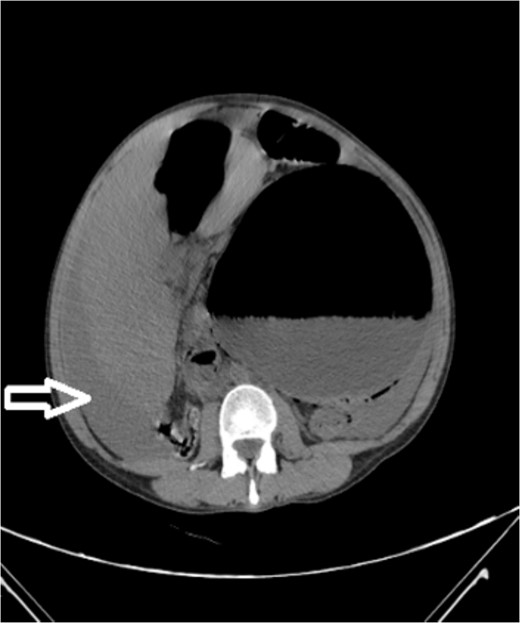
Noncontrast axial CT scan of the abdomen showing a perihepatic hematoma.
During the intraoperative exploration, large amounts of dark blood with clots were found in the abdominal cavity. An ectopic spleen was observed in the right upper abdominal quadrant, along with congested splenic and gastric veins. A 10-cm splenic laceration was noted on the anterior splenic surface, although there was no active bleeding. Additionally, ecchymosis was present on the outer gastric surface near the fundus. Given the identification of the splenic laceration in this hemodynamically unstable patient, a splenectomy was performed. An upper gastrointestinal endoscopy conducted in the operating room revealed an area of clotted blood and congestion corresponding to the area near the fundus, with no active bleeding noted. Postoperatively, the patient was transferred to the intensive care unit, where she experienced an uncomplicated recovery. A follow-up was arranged in the outpatient clinic, and she was referred for postsplenectomy vaccination.
Discussion
Wandering spleen is an uncommon clinical entity where the spleen lacks its usual peritoneal attachments, allowing it to migrate within the abdomen, predisposing it to a variety of complications. The most severe of these include torsion and infarction, but laceration, particularly post-trauma, is a critical concern as demonstrated in our case [7]. Splenic laceration in a wandering spleen, such as observed in our postpartum patient, is a rare complication that significantly complicates clinical management due to its atypical presentation and the challenges it presents in timely diagnosis.
The most common complication of wandering spleen is torsion. Other nontraumatic complications include splenic infarction, splenic abscess, variceal hemorrhage, and pancreatic tail necrosis. These complications can occur unexpectedly, emphasizing the need for a high index of suspicion and early intervention [8]. Traumatic complications and challenges associated with wandering spleen involve splenic rupture and hemorrhage, which necessitate prompt surgical intervention [9]. Surgical indications for wandering spleen primarily include symptomatic cases, those with evidence of torsion, or complications. However, there are instances where patients with asymptomatic wandering spleen might be managed conservatively with regular monitoring and follow-up, but the complications rate is 65% [10].
Similar cases have noted that delayed diagnosis of wandering spleen injury is common, often resulting in increased morbidity due to progression toward splenic rupture or significant hemorrhage. For instance, a case of a 5-year-old girl with traumatic rupture of a wandering spleen reported by Horwitz and Black indicates that even minor trauma can precipitate severe outcomes in patients with this anatomical anomaly [9]. This aligns with our observation where the postpartum state, possibly contributing to further ligamentous laxity, and a minor fall led to significant splenic injury. In another case, spontaneous volvulus of the splenic pedicle with an infarcted spleen necessitated a splenectomy, which was performed on a 44-year-old man who presented with an acutely distended and rigid abdomen [11]. This indicates that a wandering spleen is a serious condition that can lead to complications unexpectedly, even without prior trauma. It is recommended that surgical intervention be considered even for asymptomatic patients, due to the high risk of complications (65%) if the mass is not removed [12].
The epidemiology of wandering spleen remains poorly understood, but it is particularly noteworthy in women of reproductive age and in pediatric populations, where it may initially present with nonspecific symptoms or be discovered incidentally during imaging for unrelated conditions [13]. The laxity of ligaments, possibly exacerbated by hormonal changes during pregnancy or postpartum, may add to the risk of displacement and subsequent complications.
In the diagnosis of wandering spleen, noncontrast-enhanced CT scans are invaluable, especially in emergent settings where contrast use may be avoided due to patient instability or renal impairment [14]. In our case, the use of noncontrast CT was pivotal in identifying the ectopic location of the spleen and the extent of the hematoma, although it limited detailed assessment of vascular structures. Nonetheless, we opted for a contrast-free scan due to the patient’s instability.
Moreover, while there is currently a lack of studies addressing the follow-up and monitoring of patients with a wandering spleen prior to surgical intervention, it is crucial to emphasize the importance of preventive measures and early detection strategies. Regular follow-up and imaging in patients known to have wandering spleen could potentially prevent severe complications by monitoring changes in spleen position or early signs of vascular compromise.
Management strategies for wandering spleen with complications such as laceration or torsion typically involve surgical intervention, given the high risk of morbidity associated with nonoperative management. Both splenopexy and splenectomy are described in the literature; however, the choice largely depends on the spleen’s viability and the patient’s hemodynamic stability [15]. In our case, the decision for splenectomy was driven by the extensive laceration and the inability to perform vascular salvage procedures, a decision supported by other documented cases where splenic preservation was not feasible. The choice of surgical approach should be tailored to each patient, considering factors such as age, overall health, and future risk of complications.
Conclusion
This case illustrates the diagnostic and management challenges of delayed presentation of splenic laceration in a postpartum patient with a wandering spleen after trauma. Timely recognition is often aided by a CT scan with contrast. However, in this patient’s clinical course, a noncontrast CT scan was obtained, revealing hemoperitoneum and a wandering spleen. There was concern for splenic injury in the hemodynamically unstable patient. This finding was sufficient to take the patient to the operating room without the need for a contrast-enhanced CT scan. While there is no standardized preoperative monitoring protocol, proactive surveillance may help mitigate complications. Surgical treatment, tailored to each patient’s condition, remains the mainstay, with splenopexy or splenectomy depending on spleen viability and patient stability. This highlights the necessity for clinical vigilance and individualized approaches in managing wandering spleen-related complications, especially post-trauma.
Author contributions
Ahmad Awwad, Abdalhakim Shubietah (Conceptualization) and Alaa Zayed, Enas Samara, Abdalhakim Shubietah (Writing—review and editing). All authors contributed to the composition of the original draft and participated in the literature search.
Conflict of interest statement
None declared.
Funding
None declared.
Ethical approval
Ethical approval is exempt/waived at our institution.
Consent
The patient provided written consent for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal upon request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Guarantor
Abdalhakim Shubietah.



