-
PDF
- Split View
-
Views
-
Cite
Cite
Nguyen Viet Anh, Nguyen Thi Khanh Ly, Hoang Viet, Anand Marya, Correction of a severe post-surgical iatrogenic class II anterior open bite with lingual appliances and mini-screws: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae496, https://doi.org/10.1093/jscr/rjae496
Close - Share Icon Share
Abstract
An iatrogenic open bite after orthognathic surgery is an uncommon malocclusion, with only one documented case reported in the literature. However, the open bite in this case report was not a true open bite, as it resulted from the interferences between the maxillary second molars and mandibular retromolar bones. This case report aims to present the management of a true iatrogenic open bite with posterior teeth in centric occlusion, occurring after mandibular setback surgery. The anterior open bite accompanied a severe class II malocclusion and increased lower anterior facial height. The patient was treated with fixed lingual appliances and mini-screws to distalize the entire maxillary arch and close the open bite. After treatment, a positive overbite and dental class I relationship was achieved. The treatment outcomes were stable at the 2-year follow-up. Lingual appliances combined with mini-screws may offer effective non-surgical management of iatrogenic open bite after orthognathic surgery.
Clinical and Surgical Implications: Iatrogenic open bites can develop from various causes that include surgical options such as orthognathic surgery or in patients treated with occlusal splint therapy. These may be treated with the help of skeletal anchorage options such as orthodontic mini-screws.
Introduction
An anterior open bite is defined as a malocclusion characterized by the absence of contact between the anterior teeth at maximal inter-cuspal occlusion. The aetiology of anterior open bites may be multifactorial, involving heredity and environmental factors, or more straightforward causes such as oral habits, pathologic diseases, or dental treatment [1, 2]. Orthodontic management of anterior open bite is considered challenging, with a high relapse tendency, especially in cases of skeletal vertical excess [3].
Iatrogenic open bites may occur secondarily to occlusal splint therapy, deficient orthodontic retainers, or orthognathic surgery [3–5]. Among the published studies, splint therapy is identified as the most common cause of iatrogenic open bites [6]. There is only one case report presenting an iatrogenic open bite after orthognathic surgery which was not a true open bite but rather a result of interference between the maxillary second molars and mandibular retromolar bones [5].
This case report aims to present the management of a true iatrogenic open bite with posterior teeth in centric occlusion, occurring after mandibular setback surgery.
Case presentation
A 28-year-old patient presented with a chief complaint of anterior open bite, occurring immediately after bilateral sagittal split mandibular setback osteotomy. Before the orthognathic surgery, the patient had a severe skeletal class III malocclusion due to a prognathic mandible. The surgery was performed by a plastic surgeon instead of a maxillofacial one, without comprehensive orthodontic–orthognathic treatment planning 1 year prior. Post-surgery, the anterior open bite developed and gradually increased in severity. Her medical, family, and psycho-social history were non-contributory.
On an extraoral evaluation, the patient had a slightly increased lower anterior facial height with a right deviated mandible (Fig. 1). The lateral view showed a flat profile with a normal nasolabial angle. No sign of a temporomandibular joint disorder was detected.

On intraoral evaluation, the patient had full-cusp class II molar and canine relationships on the right side and end-on class II molar and canine relationships on the left side. The anterior teeth and first premolars were in an open bite with an overbite of −3.1 mm. There was mild crowding of 1.2 mm in both arches. The upper dental midline was found to be deviated 1 mm to the left.
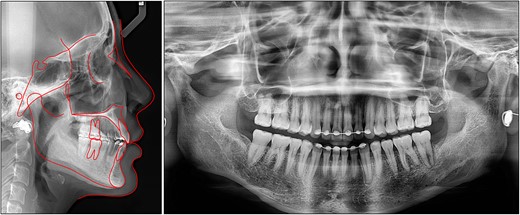
On a lateral cephalometric evaluation, the patient had a skeletal class I relationship (point A-nasion-point B angle, 4.0°) with a hyperdivergent facial pattern (Frankfort mandibular angle, 32.5°) (Table 1). The panoramic radiograph showed the presence of all teeth including the third molars (Fig. 2). The patient was diagnosed with an iatrogenic open bite and class II malocclusion on a skeletal class I relationship.
| . | Pretreatment . | Posttreatment . | Norm . |
|---|---|---|---|
| Skeletal | |||
| SNA (°) | 81.3 | 81.0 | 81.1 ± 3.7 |
| SNB (°) | 77.3 | 77.9 | 79.2 ± 3.8 |
| ANB (°) | 4.0 | 3.1 | 2.5 ± 1.8 |
| FMA (°) | 32.5 | 31.0 | 25.0 ± 4.0 |
| SN-MP (°) | 39.2 | 37.7 | 32.0 ± 6.0 |
| Dental | |||
| Upper incisor/SN (°) | 99.5 | 98.4 | 105.3 ± 6.6 |
| Upper incisor/NA (°) | 18.2 | 17.7 | 22.0 ± 5.0 |
| Upper incisor/NA (mm) | 4.4 | 2.6 | 4.0 ± 3.0 |
| Lower incisor/MP (°) | 83.8 | 90.5 | 90.0 ± 3.5 |
| Lower incisor/NB (°) | 20.2 | 27.0 | 25.0 ± 5.0 |
| Lower incisor/NB (mm) | 4.5 | 4.3 | 4.0 ± 2.0 |
| Interincisal angle (°) | 137.6 | 132.1 | 128.0 ± 5.3 |
| Upper incisal display (mm) | 0.6 | 1.0 | 2.5 ± 1.5 |
| Overjet (mm) | 5.8 | 2.1 | 2.0 ± 2.0 |
| Overbite (mm) | −3 | 1.2 | 2.0 ± 2.0 |
| Soft tissue | |||
| E-line/Upper lip (mm) | −2.3 | −1.7 | 0.0 ± 2.0 |
| E-line/Lower lip (mm) | −1.7 | −1.1 | 0.0 ± 2.0 |
| . | Pretreatment . | Posttreatment . | Norm . |
|---|---|---|---|
| Skeletal | |||
| SNA (°) | 81.3 | 81.0 | 81.1 ± 3.7 |
| SNB (°) | 77.3 | 77.9 | 79.2 ± 3.8 |
| ANB (°) | 4.0 | 3.1 | 2.5 ± 1.8 |
| FMA (°) | 32.5 | 31.0 | 25.0 ± 4.0 |
| SN-MP (°) | 39.2 | 37.7 | 32.0 ± 6.0 |
| Dental | |||
| Upper incisor/SN (°) | 99.5 | 98.4 | 105.3 ± 6.6 |
| Upper incisor/NA (°) | 18.2 | 17.7 | 22.0 ± 5.0 |
| Upper incisor/NA (mm) | 4.4 | 2.6 | 4.0 ± 3.0 |
| Lower incisor/MP (°) | 83.8 | 90.5 | 90.0 ± 3.5 |
| Lower incisor/NB (°) | 20.2 | 27.0 | 25.0 ± 5.0 |
| Lower incisor/NB (mm) | 4.5 | 4.3 | 4.0 ± 2.0 |
| Interincisal angle (°) | 137.6 | 132.1 | 128.0 ± 5.3 |
| Upper incisal display (mm) | 0.6 | 1.0 | 2.5 ± 1.5 |
| Overjet (mm) | 5.8 | 2.1 | 2.0 ± 2.0 |
| Overbite (mm) | −3 | 1.2 | 2.0 ± 2.0 |
| Soft tissue | |||
| E-line/Upper lip (mm) | −2.3 | −1.7 | 0.0 ± 2.0 |
| E-line/Lower lip (mm) | −1.7 | −1.1 | 0.0 ± 2.0 |
SNA, sella-nasion-point A; SNB, sella-nasion-point B; ANB, point A-nasion-point B; FMA, Frankfort mandibular angle; SN-MP, sella-nasion to mandibular plane; SN, sella-nasion; NA, nasion-point A; MP, mandibular plane; NB, nasion-point B.
| . | Pretreatment . | Posttreatment . | Norm . |
|---|---|---|---|
| Skeletal | |||
| SNA (°) | 81.3 | 81.0 | 81.1 ± 3.7 |
| SNB (°) | 77.3 | 77.9 | 79.2 ± 3.8 |
| ANB (°) | 4.0 | 3.1 | 2.5 ± 1.8 |
| FMA (°) | 32.5 | 31.0 | 25.0 ± 4.0 |
| SN-MP (°) | 39.2 | 37.7 | 32.0 ± 6.0 |
| Dental | |||
| Upper incisor/SN (°) | 99.5 | 98.4 | 105.3 ± 6.6 |
| Upper incisor/NA (°) | 18.2 | 17.7 | 22.0 ± 5.0 |
| Upper incisor/NA (mm) | 4.4 | 2.6 | 4.0 ± 3.0 |
| Lower incisor/MP (°) | 83.8 | 90.5 | 90.0 ± 3.5 |
| Lower incisor/NB (°) | 20.2 | 27.0 | 25.0 ± 5.0 |
| Lower incisor/NB (mm) | 4.5 | 4.3 | 4.0 ± 2.0 |
| Interincisal angle (°) | 137.6 | 132.1 | 128.0 ± 5.3 |
| Upper incisal display (mm) | 0.6 | 1.0 | 2.5 ± 1.5 |
| Overjet (mm) | 5.8 | 2.1 | 2.0 ± 2.0 |
| Overbite (mm) | −3 | 1.2 | 2.0 ± 2.0 |
| Soft tissue | |||
| E-line/Upper lip (mm) | −2.3 | −1.7 | 0.0 ± 2.0 |
| E-line/Lower lip (mm) | −1.7 | −1.1 | 0.0 ± 2.0 |
| . | Pretreatment . | Posttreatment . | Norm . |
|---|---|---|---|
| Skeletal | |||
| SNA (°) | 81.3 | 81.0 | 81.1 ± 3.7 |
| SNB (°) | 77.3 | 77.9 | 79.2 ± 3.8 |
| ANB (°) | 4.0 | 3.1 | 2.5 ± 1.8 |
| FMA (°) | 32.5 | 31.0 | 25.0 ± 4.0 |
| SN-MP (°) | 39.2 | 37.7 | 32.0 ± 6.0 |
| Dental | |||
| Upper incisor/SN (°) | 99.5 | 98.4 | 105.3 ± 6.6 |
| Upper incisor/NA (°) | 18.2 | 17.7 | 22.0 ± 5.0 |
| Upper incisor/NA (mm) | 4.4 | 2.6 | 4.0 ± 3.0 |
| Lower incisor/MP (°) | 83.8 | 90.5 | 90.0 ± 3.5 |
| Lower incisor/NB (°) | 20.2 | 27.0 | 25.0 ± 5.0 |
| Lower incisor/NB (mm) | 4.5 | 4.3 | 4.0 ± 2.0 |
| Interincisal angle (°) | 137.6 | 132.1 | 128.0 ± 5.3 |
| Upper incisal display (mm) | 0.6 | 1.0 | 2.5 ± 1.5 |
| Overjet (mm) | 5.8 | 2.1 | 2.0 ± 2.0 |
| Overbite (mm) | −3 | 1.2 | 2.0 ± 2.0 |
| Soft tissue | |||
| E-line/Upper lip (mm) | −2.3 | −1.7 | 0.0 ± 2.0 |
| E-line/Lower lip (mm) | −1.7 | −1.1 | 0.0 ± 2.0 |
SNA, sella-nasion-point A; SNB, sella-nasion-point B; ANB, point A-nasion-point B; FMA, Frankfort mandibular angle; SN-MP, sella-nasion to mandibular plane; SN, sella-nasion; NA, nasion-point A; MP, mandibular plane; NB, nasion-point B.

The surgical treatment option was refused by the patient, therefore a non-surgical treatment plan was selected to distalize the entire maxillary arch for correcting the class II malocclusion and intrude the maxillary molars for closing the open bite. Due to the severity of the open bite and class II malocclusion, the patient was counselled about the possibility of future surgical intervention if orthodontic treatment alone was insufficient to address the issues.
Clinical procedures and outcomes
The patient’s dentition was bonded with 0.018″ × 0.025″ lingual appliances (DLB, Dentos, Korea) and vacuum-formed indirect bonding trays [7]. After 4 months of initial levelling and alignment, two mini-screws (diameter, 1.6 mm; length 10 mm; Medico, Korea) were implanted into the palate between the maxillary first and second molars. The entire maxillary arch was distalized with a retraction force of 200 g on each side from the mini-screws. The rationale was to correct the class II anteroposterior relationship and rotate the upper arch clockwise for intruding the maxillary molars and extruding the maxillary incisors (Fig. 3) [8].

After 8 months of distalization, class I canine and molar relationships were obtained. To address the overbite by posterior intrusion of maxillary molars, two additional mini-screws were implanted into the buccal alveolar bone between the maxillary first and second molars (Fig. 4). The total treatment time was 19 months.

After treatment, class I canine and molar relationships were obtained on both sides with a normal overjet and positive overbite (Fig. 5). The posttreatment lateral cephalometric evaluation showed an improvement in both anteroposterior (point A-nasion-point B angle, 3.1°) and vertical dimensions (Frankfort mandibular angle, 31.0°). The posttreatment panoramic radiograph showed adequate root parallelism without any sign of root resorption (Fig. 6). The lateral cephalometric superimpositions confirmed the intrusion of the maxillary molars, the extrusions of the incisors, and the counter-clockwise autorotation of the mandible (Fig. 7).

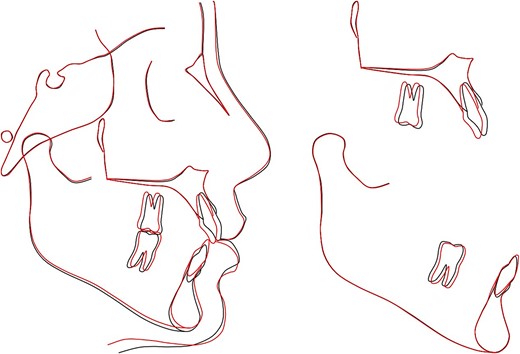
Overall and regional cephalometric superimpositions: black, pretreatment; red, posttreatment.
Bonded lingual retainers were placed in both arches along with clear retainers for night-time use. The patient was evaluated at a 2-year follow-up and the treatment results remained stable (Fig. 8). The patient expressed satisfaction with the treatment, citing both the resolution of the chief complaint and the invisible nature of the appliances.

Discussion
Iatrogenic open bites can develop from various causes, including orthognathic surgery complications or occlusal splint therapy [3–5, 9–11]. A comprehensive orthodontic treatment plan is necessary to address the open bite and the accompanying class II malocclusion. However, even with properly designed appliances, one of the main side effects of occlusal splint therapy is an irreversible change to occlusion, including anterior open bites [6, 12].
Orthodontic management of open bites may be favourable with lingual appliances as the tongue thrust habit is limited by the appliances [2, 13]. Albertini et al. [14] and Le Keux and Frapier [3] reported open bite cases addressed with this approach, the latter including logopedic therapy. However, in cases with excessive mandibular plane angles and protrusion, premolar extraction and mini-screws may become necessary, as reported by Bian et al. [15].
In this case report, the patient exhibited an iatrogenic anterior open bite, class II dental relationship, hyperdivergent facial pattern, and a well-balanced profile. Therefore, a non-extraction treatment strategy (except the third molars) combined with mini-screws was selected. The open bite was completely resolved during the vertical correction stage through maxillary molar intrusion.
Conclusion
Lingual appliances combined with mini-screws may offer effective non-surgical management of iatrogenic open bite after orthognathic surgery. In case of an anterior open bite associated with a class II malocclusion, the anteroposterior discrepancy should be addressed prior to final vertical correction.
Conflict of interest statement
The author declares no competing interests.
Consent for publication
Written informed consent for publication was obtained from the patient.



