-
PDF
- Split View
-
Views
-
Cite
Cite
Trond Kjeseth, Pål-Dag Line, Ammar Khan, Jon M Solheim, Ida G Bjørk, Jon Sundal, Mogens Jensenius, Sheraz Yaqub, Ex-situ liver resection for complex Echinococcus multilocularis infection: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 6, June 2024, rjae410, https://doi.org/10.1093/jscr/rjae410
Close - Share Icon Share
Abstract
Echinococcus multilocularis, the fox dwarf tapeworm, causes alveolar echinococcosis (AE), a critical and life-threatening condition. A radical surgical approach represents the only curative option. In this case study, we present a 37-year-old man diagnosed with extensive hepatic AE requiring ex-situ extended right-sided liver resection including the caudate lobe and retro-hepatic vena cava. The left liver segments were auto-transplanted with reconstruction of the left hepatic vein and an inferior vena cava graft. In the post-operative course, the patient developed a bile leak, which was successfully managed with endoscopic stent intervention. He was discharged after a three-week hospitalization. Medical treatment with albendazole was initiated preoperatively and continued postoperatively.
Introduction
Echinococcosis, a parasitic zoonosis in humans, ensues from the invasion by larval stages of taeniid cestodes belonging to the genus Echinococcus. The liver is the major site of echinococcosis [1]. Echinococcus multilocularis, the fox dwarf tapeworm, causes alveolar echinococcosis (AE), wherein the larval aggregation resembles a malignancy in both appearance and behaviour. It perpetuates through exogenous budding, infiltrating adjacent tissues, which is responsible for tissue destruction, and finally for liver failure and death if not optimally treated. The treatment of E. multilocularis requires an aggressive surgical approach in combination with long-term medical treatment with albendazole in order to prevent recurrence and further spread to other organs [2]. The prognosis is dismal in untreated or inadequately treated patients with AE [3]. AE is a rare condition, which is endemic in the Northern hemisphere, including North America and several Asian and European countries. In the Scandinavian countries, the incidence is exceedingly low and is almost exclusively seen as imported cases from endemic regions [4].
We report a 37-year-old healthy man with extensive liver involvement from AE that also included the retro-hepatic vena cava. Curative surgery was possible with ex-situ liver resection, vascular reconstruction and auto transplantation of the liver remnant.
Case report
A 37-year-old man from the Baltic states was referred to our hospital due to mild upper abdominal discomfort and increasing fatigue. He had no known comorbidities. His vital signs were within normal ranges. Over the past 6–7 years, he had developed a mild anaemia. Notably, C-reactive protein level was elevated at 36 mg/L (0–5 mg/L), and the Erythrocyte Sedimentation Rate was 34 mm/h (2–15 mm/h). Other blood tests, including liver function tests and tumour markers Carcinoembryonic Antigen, Cancer Antigen 19-9 and Alpha Fetoprotein, were within normal limits. Clinical examination revealed low-grade tenderness in the right upper quadrant. Abdominal computed tomography and magnetic resonance imaging of the liver unveiled a large multifocal, microcystic tumour in the liver, affecting all segments of the right hemi-liver (segments 5–8) as well as segments 1 and 4 (Fig. 1). Furthermore, there was involvement of the retro-hepatic inferior vena cava (IVC), right- and middle hepatic veins (affecting the venous outflow for liver segments 2, 3 and 4), and right portal vein. AE was suspected, and serological tests confirmed antibodies against E. multilocularis. As soon as the diagnosis was established, medical treatment with albendazole 600-mg BD was initiated.
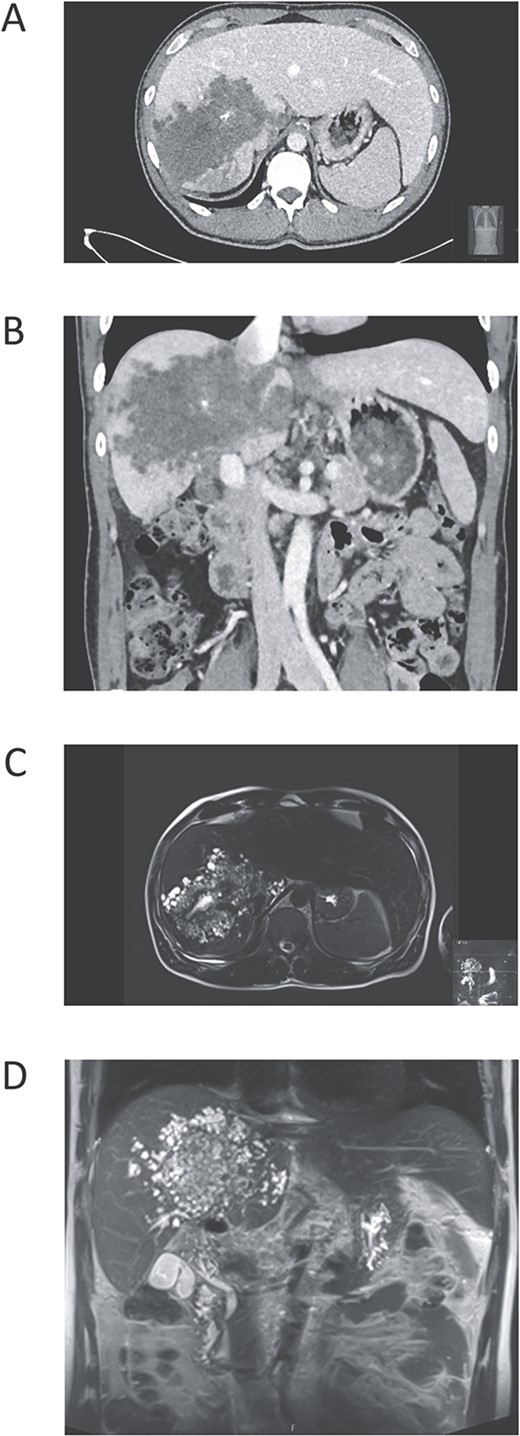
Pre-operative images of the liver. (A) Contrast-enhanced computed tomography (CT) in axial plane demonstrating a large irregular tumour mass, with central calcifications, in all segments of the right liver lobe and also affecting liver segments 1 and 4. (B) CT in coronal plane illustrating that the mass surrounds vena cava inferior. (C) Magnetic resonance imaging (MRI) T2-weighted in transversal plane depicts the typical features of Echinococcus multilocularis as a microcystic mass. (d) MRI T2-weighted image in coronal plane showing both the microcystic appearance of the tumour and also visualizing the localization above the gallbladder and the extrahepatic bile ducts.
As surgical resection is the sole curative option in AE, the patient was immediately referred to a tertiary hepatobiliary surgical unit. Due to the extensive vascular involvement, an ex-situ resection with en-bloc IVC resection was planned to prevent spillage of any infective tissue/fluids in the operation field, and allow optimal condition for vascular reconstruction. The left liver was fully mobilized, but the right lobe had dense adhesions to the diaphragm and the surrounding tissue. The hilar structures were completely dissected. Due to limited mobility, the future liver remnant (FLR), consisting of segments 2 and 3 and parts of segment 4, was first dissected free as in case of living donor hepatectomy. Due to affection of the left veno-caval confluence, the left hepatic vein was cut within the parenchyma about 3 cm from the IVC, and the FLR was taken to the back-table for ex-situ perfusion with ILG-1. A temporal portocaval shunt was created to maintain splanchnic venous flow during the anhepatic phase. The IVC was cross-clamped over and under the liver, and a venovenous bypass was established via percutaneously inserted catheters in the jugular and femoral vein as in a classic liver transplant procedure. Subsequently, the remainder EA-affected liver was taken out ‘en-bloc’ with the IVC. A blood type compatible allogeneic iliac vein was used to reconstruct the two main branches of the left hepatic vein, which thereafter were implanted into a 22-mm Dacron graft acting as an IVC replacement (Fig. 2). The liver was then auto-transplanted with classical bi-caval anastomosis (Fig. 3). The portal and arterial anastomosis were constructed using standard technique whereas the biliary drainage was reconstructed by a Roux-en-Y loop. The liver was reperfused after 207 minutes of cold ischemia. The patient was hemodynamically stable throughout the procedure. In the post-operative phase, the patient developed a bile leak, which was successfully managed with a balloon enteroscopy and transluminal stenting [5]. Following a 3-week hospitalization, the patient was discharged. The final pathology report confirmed E. multilocularis infection in the liver. The patient is prescribed albendozole for a minimum of 2 years and will undergo regular radiological monitoring and serologic testing for the next 5 years. If a recurrence occurs, the treatment with albendazole will be for an indefinite duration.

Back-table surgery on the future liver remnant (segments 2 and 3) with reconstruction of the left hepatic vein using an allograft and the retrohepatic part of inferior vena cava is reconstructed with a Dacron graft.
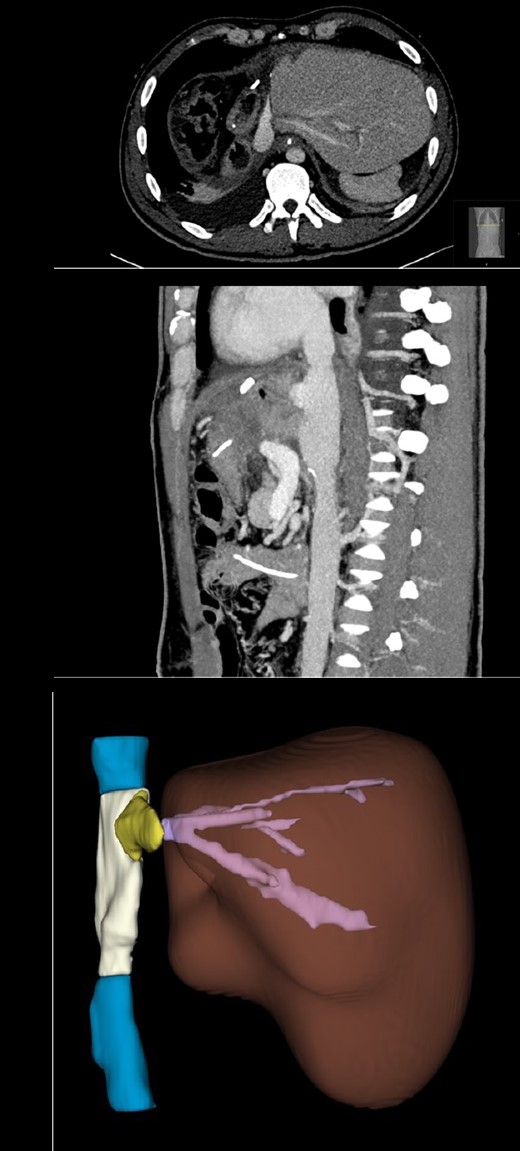
Computed tomography taken 4 weeks postoperatively. (A) CT in axial plane showing the liver remnant (segments 2 and 3) and parts of the Dacron graft in the inferior vena cava position, the left hepatic vein graft and one of the native hepatic veins of the liver. (B) CT in sagital plane showing the Dacron graft replacing the retro-hepatic inferior vena cava and the bi-caval anastomoses of the auto-transplanted liver. (C) A 3D reconstruction of the post-operative liver remnant and the iliac vein allograft (yellow) from the left hepatic veins (pink), and the inferior vena cava (blue) with the Dacron graft (white).
Discussion
Humans constitute an accidental host for E. multilocularis and are infected through the ingestion of eggs. The oncospheres infiltrate the intestinal wall and are subsequently transported through the portal circulation to the liver. Although the liver is the most frequently affected site, affection of other organs, such as lungs, kidneys, spleen, muscle and brain, is occasionally seen. Direct contact with infected foxes or consumption of contaminated berries or mushrooms are principal ways of infection [6]. The majority of cases with AE reported in Norway are in foreigners from endemic regions, as observed in the presented case. The prevailing clinical presentation involves focal pain, weight loss and/or jaundice. However, subtle symptoms, akin to those exhibited by our patient, are noted in approximately 30% of cases.
Management of AE requires a multidisciplinary approach with the aim to achieve complete resection of the infected tissue. Left untreated, E. multilocularis infection is lethal, and radical surgical resection is the only curative option. In addition to establishing the diagnosis based on radiological and serological assessment, the work-up should ascertain the resectability of the disease and the patient’s capability to undergo surgery. As exemplified in our case, extensive surgical interventions, such as ex-situ liver resection with auto-transplant, may represent the sole curative option in certain cases, and have been reported with high success rate from Chinese centres [7, 8]. However, this approach requires a physically fit patient with the disease localized exclusively in the liver. In situations where liver resection is not feasible, allogeneic liver transplant has been documented as a life-saving procedure in rare cases of AE affecting the liver.
Our case demonstrates that ex-situ liver resection with vascular reconstruction is feasible in highly selected cases of severe AE in the liver. This mandates a specialized surgical team with hepatobiliary and liver transplant skills and experience with ex-situ surgery.
Conflict of interest statement
None declared.
Funding
None declared.
References
- stents
- albendazole
- biliary leak
- hepatic resection
- reconstructive surgical procedures
- surgical procedures, operative
- tissue transplants
- inferior vena cava
- vena cava
- infections
- liver
- dwarf tapeworm
- echinococcus multilocularis infections
- echinococcus multilocularis
- bile leak
- left hepatic vein
- medical management



