-
PDF
- Split View
-
Views
-
Cite
Cite
Karen Aguirre Flores, Ulises E Mazariegos Gutiérrez, Rogelio A Blaz Zavala, Samuel R Gómez Arenas, Giant diaphragmatic hernia surgical treatment by laparoscopic repair: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 6, June 2024, rjae387, https://doi.org/10.1093/jscr/rjae387
Close - Share Icon Share
Abstract
Diaphragmatic hernias occur in up to 10%–50% of the general population. Treatment of hiatal hernias depends on the type of hernia and the severity of the symptoms. We report the case of a 52-year-old woman with no significant history who presented for 1 year with non-specific chest pain, dyspnea, dysphagia, and heartburn. A thoracoabdominal tomography with contrast was performed, showing a diaphragmatic hernia containing the stomach, portions of the duodenum, pancreas, small intestine, and colon with a sac of up to 20 cm, which was successfully repaired laparoscopically.
Introduction
Diaphragmatic hernias occur in up to 10%–50% of the general population. Among these, hiatal hernias are the most common. The giant hiatal hernia (Type IV) is one that contains at least 30% of the stomach in the thorax or even other abdominal organs, such as the colon, small intestine, omentum, and liver. These represent ~0.5% of all hiatal hernias [1, 2]. The clinical presentation includes symptoms, such as heartburn, pain in epigastrium, and chest pain, among others. The importance of its approach and treatment is that up to 30% will present with torsion and ischemia of the herniated segment, with a high mortality rate [3, 4]. In this case, we report a giant type IV hiatal hernia, which was laparoscopically repaired without complications.
Case report
The case is reported of a 52-year-old woman, without significant illnesses, who presented with non-specific chest pain for 1 year, 6 months later with intermittent episodes of dyspnea with great and medium exertion, dysphagia, and heartburn. During the examination, hypoventilated lung fields at the bases, peristaltic sounds, and tympanism on percussion were heard. The thoracoabdominal tomography with contrast shows a diaphragmatic hernia containing the stomach, portions of the duodenum, pancreas, small intestine, and colon (Fig. 1), with a sac measuring up to 20 cm (Fig. 2).
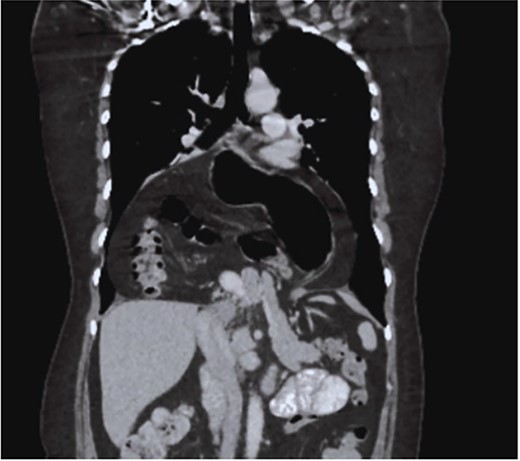
CT coronal section, showing the presence of the stomach, duodenum, small intestine, colon, and pancreas.
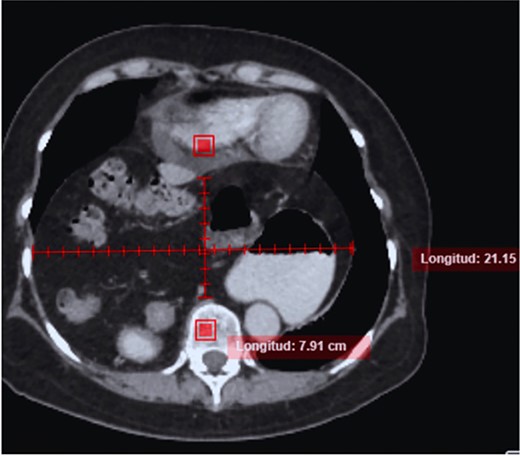
CT in axial section, hernia sac measuring ~21 × 15 × 7 cm is observed.
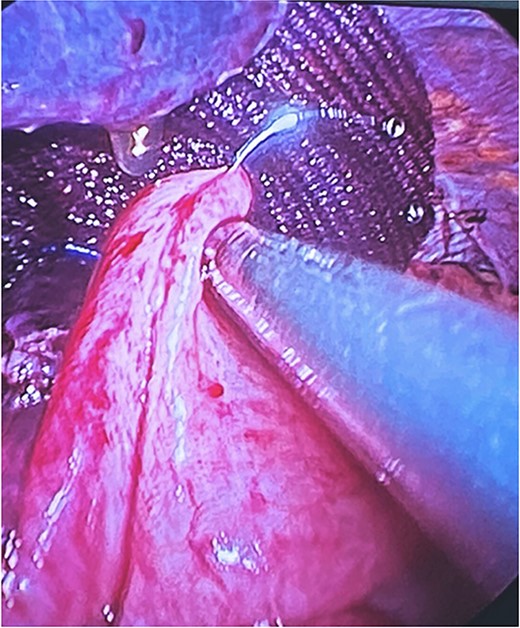
Surgical treatment was decided. Five ports were used: one supraumbilical 12 mm port for the telescope, one 5 mm subxiphoid port for the liver retractor, and three working ports placed in the left midclavicular line of 12 mm, the left axillary line of 5 mm, and the right midclavicular line of 5 mm. A type IV hiatal hernia was found with a 12 cm hernia defect (Fig. 3), a hernia sac measuring 20 cm × 15 cm × 7 cm, containing the entire stomach, dudodenum, pancreas, greater omentum, and transverse colon. The content was reduced to subsequently dissect and resect the hernia sac (Fig. 4).
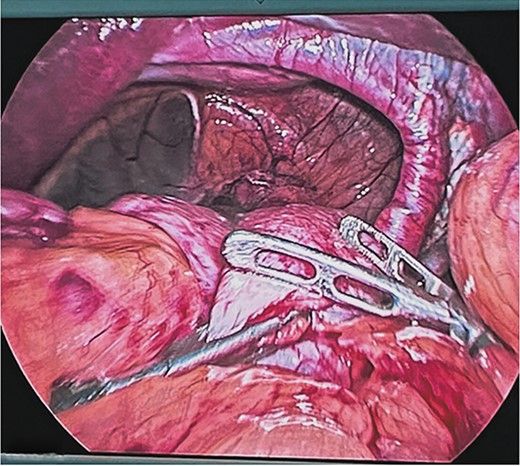
Reduction of the contents of the hernial sac with intestinal forceps and blunt dissection. Hiatal defect of ~12 cm.
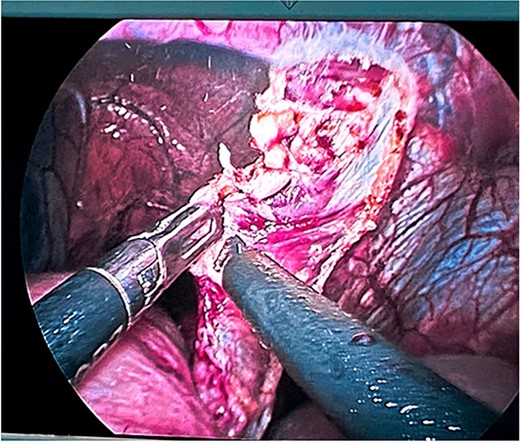
Dissection and resection of hernial sac with traction and monopolar energy.
At the end of the dissection of both diaphragmatic crura, their plasty was performed by placing six single 2-0 polypropylene suture stitches with an atraumatic needle with extracorporeal knots at both ends of the hiatus, reducing its size to 5 cm. Subsequently, a composite mesh with a resorbable coating was fixed with automatic laparoscopic staples, reducing the hiatus by up to 3 cm (Fig. 5). Finally, a Toupet fundoplication was performed as an anti-reflux mechanism (Fig. 6).

Placement of composite mesh with resorbable coating and fixing it with automatic titanium spiral sutures reducing the esophageal hiatus up to 3 cm.
Modeling of Toupet fundoplication with intracorporeal technique with polypropylene suture 2-0.
The patient had 2 days of post-surgical hospital surveillance with early mobilization, was discharged on the second day with tolerance to a liquid diet, and was followed up in the outpatient clinic at 7 days, 3 months, and 6 months with imaging studies in which both lung fields re-expanded without the presence of recurrences (Fig. 7), and reported total remission of symptoms.
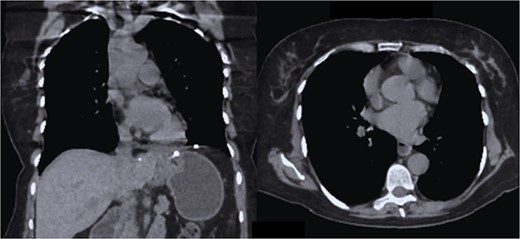
CT coronal and axial sections, showing complete re-expansion of both lung fields and the fixed mesh at the level of the hiatus esophageal without evidence of a hernia sac or recurrence.
Discussion
A hiatal hernia is a medical condition in which the upper part of the stomach or other internal organ bulges through an opening in the diaphragm.
The classification of hiatal hernias is divided into four types:
(i) Type I (sliding type), which represents >95% of hiatal hernias, occurs when the gastroesophageal junction (GEJ) is displaced upwards towards the hiatus.
(ii) Type II is a paraesophageal hiatal hernia, which occurs when part of the stomach migrates into the mediastinum parallel to the esophagus.
(iii) Type III is both a paraesophageal hernia and a sliding hernia, where both the GEJ and a portion of the stomach have migrated into the mediastinum.
(iv) Type IV is when the stomach, as well as an additional organ, such as the colon, small intestine, or spleen, also herniate into the chest [2].
The clinical presentation includes symptoms, such as heartburn, pain in epigastrium, and chest pain, among others [3, 4]. Paraesophageal hernias may present with gastric volvulus due to laxity of the peritoneal insertions of the stomach and subsequent rotation of the gastric fundus. This is considered a surgical emergency [5–7].
According to the Society of American Gastrointestinal and Endoscopic Surgeons, only investigations that will have an impact on the clinical management of the patient should be performed [8]. The diagnosis of hiatal hernia can be rather challenging at times due to the shift in the anatomy of the esophagogastric junction during deglutition, respiration, and movement. A complete history and physical exam are mandatory, as they may reveal symptoms that were not previously apparent. Current diagnostic methods for hiatal hernia are:
(i) Barium swallow X-ray: evaluates motility dysfunction, stenosis, and short esophagus diagnosis.
(ii) Endoscopy: analysis of esophageal mucosa, erosive esophagitis, Barrett’s esophagus, malignancy, Cameron’s ulcers, and swallowing difficulty.
(iii) Manometry: evaluates the integrity of esophageal peristaltis, motility disorders, and achalasia.
(iv) pH testing: quantitative analysis of reflux episodes.
(v) Computer tomography (CT): evaluates size, location of hernia, gastric volvulus, perforation, pneumoperitoneum, and pneumomediastinum [8].
Currently, the standard of surgical treatment for giant diphragmatic hernias is minimally invasive, either by laparoscopy or robot-assisted; however, it is a complex procedure, and its management is not completely standardized. Although in some systematic reviews it has been estimated that prosthetic reinforcement reduces the recurrence of hiatal hernia compared to diaphragmatic crura plasty alone, there are also reports of esophageal or gastric erosion due to the use of meshes [8, 9].
More information is still needed to standardize the treatment, while individualization of each patient is mandatory. In this case, a technique with diaphragmatic crura plasty and reinforcement with a composite mesh with a resorbable coating was decided without presenting recurrences or complications associated with its use [10, 11].
Conclusion
The standard of surgical treatment for giant diphragmatic hernias is minimally invasive with adequate evolution, as presented in our case report; however, each patient must be individualized.



