-
PDF
- Split View
-
Views
-
Cite
Cite
Yohei Kawatani, Hirofumi Saitoh, Takaki Hori, Phlegmasia cerulea dolens after endovenous cyanoacrylate closure of incompetent small saphenous vein, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjae363, https://doi.org/10.1093/jscr/rjae363
Close - Share Icon Share
Abstract
A previously healthy 70-year-old woman underwent cyanoacrylate closure of an incompetent left small saphenous vein. Six days later, grade 2 treatment-induced thrombosis occurred at the sapheno-popliteal junction. Three days later, the patient presented with pale, cold pain in the left lower extremity. Diffuse thrombosis of the left lower extremity involved the small and great saphenous and deep veins. The patient was admitted and immediately administered heparin with anticoagulant factors, with symptoms began resolving 1 d later. The superficial vein thrombi were resolved. Although a deep venous thrombus remained, symptoms disappeared, and the patient was discharged.
Introduction
Venous thrombosis is a well-known complication of endovenous ablation for treating saphenous vein insufficiency [1–3]. Endovenous ablation-induced thrombosis is also known as endovenous heat-induced thrombosis (EHIT) or endovenous glue-induced thrombosis (EGIT). However, most of these complications are mild [4]. In this study, we encountered a case of severe manifestation of venous thrombosis presenting as phlegmasia cerulea dolens (PCD) following endovenous cyanoacrylate closure (CAC) for treating small saphenous vein insufficiency.
Case presentation
A 75-year-old woman contacted the emergency medical services 9 d after undergoing CAC for bilateral small saphenous vein insufficiency and reported acute swelling, pain, and paleness in the left lower extremity.
The patient was healthy, except for presenting with hypertension and dyslipidemia. The patient had no history of deep venous thrombosis (DVT) or thrombotic predisposition.
Operative procedures were performed using a CAC device (Venaseal, Medotoronic, Dublin, Ireland), according to the manufacturer’s instructions. Ultrasound examination at the end of surgery confirmed the presence of a precise occlusion, which was 2 cm distally to the small saphenous–popliteal vein junction. Examination 6 d after surgery revealed a grade 2 EGIT, which was observed without medication.
On postoperative Day 9, the patient experienced pale, cold pain in the left lower extremity (Fig. 1a). The symptoms progressed rapidly and at 4 h after their onset, the patient could not walk because of pain and paralysis in the left lower extremity. Ultrasonography revealed total occlusion of the left deep veins from the common iliac to the popliteal vein. Moreover, occlusion was also observed in superficial veins, including the great saphenous vein (GSV) and its branches (Fig. 2a and b). Arterial ultrasound examination showed no thrombus or occluded lesion but impaired pulsatile flow in the left lower extremity. Blood tests revealed very high levels of D-dimer (25 ng/mL) and fibrinin/fibrinogen degradation products (100 μg/mL).
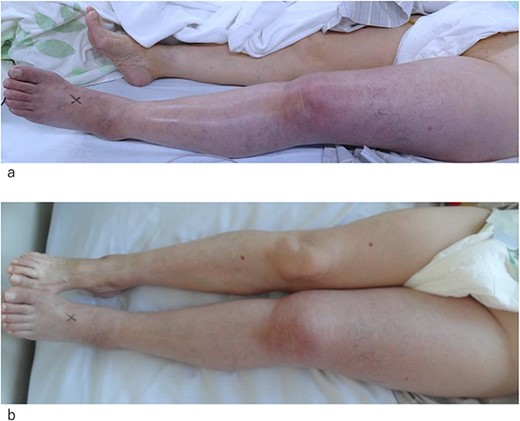
Photograph of the affected leg. (a) At the day of admission. The left leg appears pale and swollen. The superficial veins are occluded. (b) One day after admission. The color of the skin and occlusion of the superficial vein appears improved. Swelling of the leg is still observed.
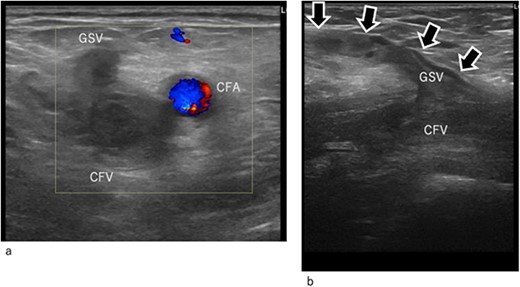
Duplex ultrasound image at arrival. (a) Transverse image. (b) Longitudinal image. The common femoral and GSV (arrow mark) are occluded by thrombi. CFA, common femoral artery; CFV, common femoral vein; GSV, great saphenous vein.
Systemic administration of heparin was initiated in the emergency room and continued in the high-care unit. Despite this, the activated clotting time was ~130 s. Suspecting a fibrinolytic protein shortage, antithrombin III agents and plasma transfusion were administered.
By Day 2 of hospitalization, the pale skin of the patient and pain started to improve, and she was able to move her left lower extremity (Fig. 1b). Enhanced computed tomography (CT) revealed the resolution of the thrombus in the GSV; however, the deep veins remained completely occluded by thrombi (Fig. 3a and b). An ultrasound arteriogram revealed normal arterial blood flow.
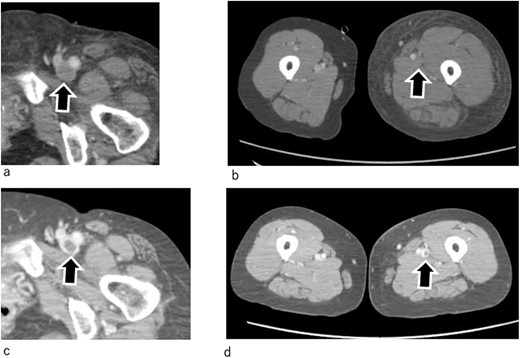
Enhanced CT. (a, b) One day after admission. The thrombus in the GSV has disappeared. However, thrombi are still observed in the deep veins, which remain totally occluded. (c, d) On Day 7. The thrombi in the deep veins have shrunk, and the veins have recanalized. Arrow marks indicate femoral veins.
On Day 9 of hospitalization, the leg swelling resolved. Contrast-enhanced CT revealed partial recovery of blood flow in the deep veins (Fig. 3c and d). In addition, the swelling of the left lower extremity resolved (Fig. 3b and d). Following this, heparin was changed to the oral anticoagulant apixaban (10 mg/d).
Although a deep venous thrombus remained in the common iliac vein to the superficial femoral vein, the left lower extremity swelling resolved. The patient was discharged asymptomatic.
Discussion
EGITs are common [1–3]; however, most EGITs are not associated with clot extension or migration [2, 4]. In patients with grade 1 or 2 EGITs, administration of anticoagulant or antiplatelet agents is considered unnecessary because these typically resolve on their own, as previously observed [2, 3].
In our case, only grade 2 EGIT was noted on postoperative Day 6; however, 3 d later, the patient experienced the most severe manifestation of venous thrombosis. The thrombus diffused into the iliac, femoral, popliteal, and GSV.
Gressenberger et al. reported a case of DVT after CAC due to glue extension into the common iliac vein [5]. In the case, the thrombus extended from the GSV to the common femoral vein near the treated area. In contrast, our patient experienced broad thrombosis. Anatomically, the pelvic veins and GSV are not near the treated vein. Based on records and findings, the etiology was assumed to be thrombus extension caused by EGIT in the small saphenous–popliteal vein. However, this hypothesis remained unverified as simple thrombus extension affects veins far from the treated region. There is a possibility that, as Parsi et al. warned, systemic thromboembolic events may occur after CAC [1].
PCD is a rare and extreme manifestation of deep and superficial venous thrombosis that can lead to limb loss and ultimately death [6]. Extreme hypertension in veins can lead to impaired arterial blood flow, which can lead to venous gangrene if untreated [7]. Triggering factors for PCD include surgery, femoral vein catheterization, pregnancy, leg stasis, hypercoagulability, and vascular wall injury [8, 9]. A universal treatment approach for PCD has not yet been established. Currently, the initial treatment for PCD is bedrest, while intensive care includes fluid resuscitation and systemic heparin administration [10, 11]. Systemic administration of thrombolytic agents [12] or catheter-directed thrombolysis are some of the options for treating DVT [13]. Surgical resection of the thrombus is also an alternative option [14].
Post-CAC PCD is an extremely rare complication. In this case, heparin was administered along with antithrombin III agents and plasma transfusion to correct the fibrinolytic system. The superficial veins were recanalized. Consequently, the leg and life of the patient were saved. The successful outcome was attributed to the early administration of heparin after onset, which was ~4 h. The critical point of resolution in PCD is the resolution of the superficial acute thrombus. This improves venous blood flow via the superficial venous network, which resolves the low tissue perfusion caused by the occlusion. In the present case, although the deep vein occlusion persisted, the symptoms of the patient and physical findings improved.
Theoretically, PCD is established when thrombosis extends to the collateral veins, with massive fluid sequestration, greater edema, and low arterial perfusion [15]. Therefore, we assumed that thrombus formation in the collateral veins is a critical treatment goal in PCD. In this case, thrombus disappearance and symptom improvement occurred simultaneously. Despite the persisting DVT, the limb and life of the patient were rescued. Therefore, we did not perform additional radical treatment for DVT other than heparin administration followed by oral anticoagulants.
In conclusion, this case demonstrated that the critical point in PCD treatment after CAC is the immediate initiation of anticoagulation therapy to resolve thrombosis in the collateral veins.
Acknowledgements
Written informed consent for publication was obtained from all the participants. This study was approved by our institutional review board.
Author contributions
Y.K., H.S., and T.H. conducted this study and approved manuscript.
Conflict of interest statement
None declared.
Funding
Self-funded.



