-
PDF
- Split View
-
Views
-
Cite
Cite
Seidali Abdaliyev, Daniyar Yestay, Daulet Baitov, Correction of a congenital kyphoscoliosis associated with diastematomyelia, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae153, https://doi.org/10.1093/jscr/rjae153
Close - Share Icon Share
Abstract
Congenital scoliosis is one of the most common deformities of the spine in children. Intraspinal anomalies are always accompanied with congenital scoliosis. Diastematomyelia is one of the most common intraspinal pathologies in congenital scoliosis. To date, there is no standard method for correcting the congenital spinal deformity associated with diastematomyelia. We present a clinical case of simultaneous correction of congenital scoliosis by an internal corrector with excision of diastematomyelia. The patient tolerated the surgery well without any complications. She was discharged home with improved symptoms without need for additional therapy. The patient’s guardians consented to the procedure and to the publication of her image.
Introduction
Congenital scoliosis is the most common spinal deformity in children and affects ~2%–11% [1]. Congenital scoliosis is a failure of vertebral formation, segmentation, or a combination of them, arising from abnormal development of the vertebrae in the period from 4 to 6 weeks of pregnancy [2]. The prevalence of intraspinal abnormalities in congenital scoliosis ranges from 20% to 58% [3]. The most common anomalies in congenital scoliosis are syringomyelia, diastematomyelia, and a fixed spinal cord [4, 5]. Diastematomyelia (split cord malformation) is one of the variants of spinal dysraphy, when the spinal cord is divided into two arms by a septum located in the sagittal area. S.R. Olivier first described this anomaly in 1837 [6].
At the moment, there are several types of surgical correction of congenital scoliosis associated with diastematomyelia. A number of authors are supposed about the traditional, two-stage method of treatment [7, 8]. At the first stage, diastematomyelia is removed, and at the second stage, scoliosis is corrected. Other authors talk about the opportunity of a one-stage operation [9–11]. Some authors do not exclude the possibility of correction of scoliosis without resection of diastematomyelia; however, to date, this method has not been sufficiently studied and the risks of complications are very high [12]. Therefore, the choice of surgical tactics remains relevant. At the same time, simultaneous and minimally invasive interventions are a priority choice, especially for vertebral anomalies [13, 14].
The intention of this article is review with the clinical case of simultaneous surgery in a patient with congenital scoliosis on the background of failure of vertebral segmentation with diastematomyelia.
Clinical case
Patient M., female, 17 years old, was admitted to the Department of Orthopedics with a diagnosis of congenital kyphoscoliosis on the background of failure of vertebral segmentation (concretion of Th8–Th12 vertebrae): spinal cord anomaly (diastematomyelia). The patient gave written informed consent to the publication of her clinical data.
She complained of the presence of spine deformity with nagging pain in the thoracolumbar spine. According to the legal representatives, spinal deformity from birth has progressed in dynamics. She has constantly undergone courses of conservative treatment.
During the examination, the patient moves independently, there is an asymmetry of the shoulder blades, shoulder pads. Pronounced scoliotic deformity of the thoracolumbar spine is determined, the arch of the bulge is turned to the right; rib hump on the right and muscle roller on the left. Palpation is painful in the thoracolumbar spine. The Adams test is positive. Movements in the thoracolumbar spine are limited. The frontal balance of the trunk is disturbed, and sagittal balance is preserved (Fig. 1). There are no neurological disorders on the periphery of the lower extremities, and the functions of the pelvic organs are not violated.
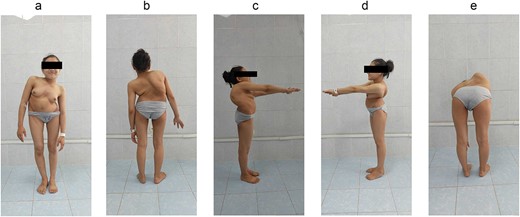
Preoperative patient’s appearance: (a) front, (b) back, (c) right side, (d) left side, and (e) the Adams test is positive.
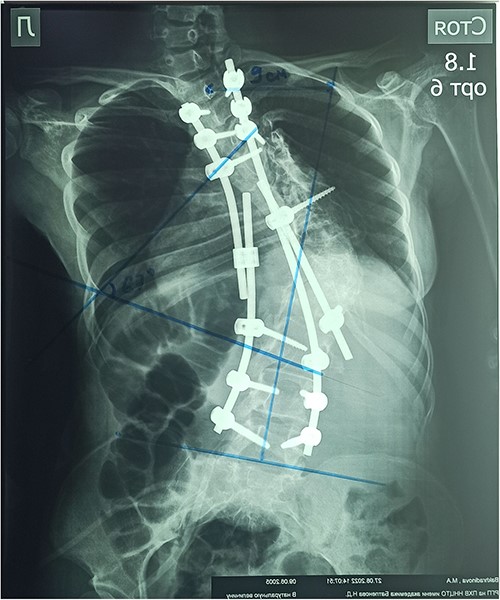
On the preoperative anterior–posterior X-ray, the Cobb angle was 110°; violation of frontal balance—13 cm (Fig. 2).
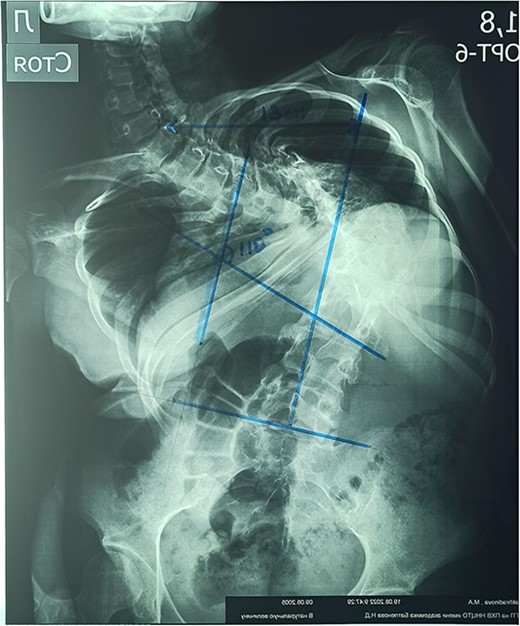
The rigidity of the scoliotic arch is noted on functional X-rays and on stretching (Fig. 3).
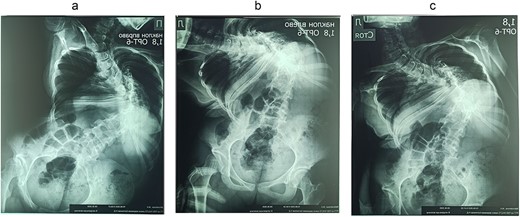
Preoperative functional X-ray: (a) inclination to the right, (b) inclination to the left, and (c) on stretching.
Magnetic resonance imaging (MRI) visualizes the separation of the spinal cord into two arms at the Th11 level (Fig. 5).

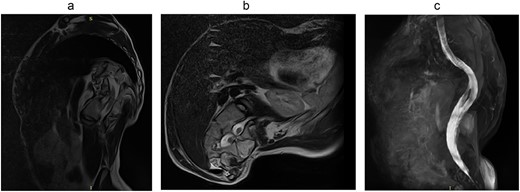
Computed tomography (CT) visualizes diastematomyelia in the form of a calcar at the level of Th11, Th12, L1 vertebrae (Fig. 4).
The patient underwent surgery: laminectomy of Th11, Th12, L1 vertebrae, partial excision of diastematomyelia, and decompression of the spinal cord; pedicular subtraction osteotomy at the level of Th9, Th10 vertebrae with resection of 11, and 12 ribs on the right side. Correction of congenital deformity and transpedicular stabilization (Medtronic, USA, no conflict interest) (Fig. 6).
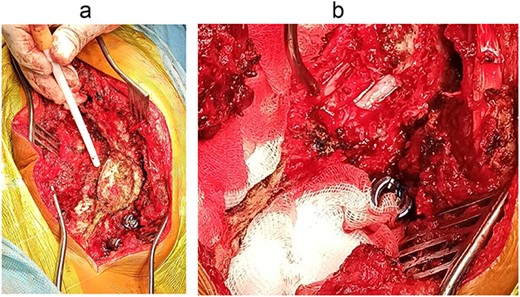
Intraoperative images: (a) splitting of spinous processes of Th11, Th12, L1 vertebrae; (b) separation of the spinal cord into two arms (indicated by arrows).
In the early postoperative period, the patient complained of moderate local pain. There were no neurological disorders on the periphery of the lower extremities. The function of the pelvic organs was normal. On the seventh day after the operation, the patient underwent a X-ray control. After surgery, the Cobb angle was 67°, the correction was 60.9%, and the frontal balance was 9 cm (Fig. 7).
The patient was released from hospital on the 10th day after the operation with good clinical result (Fig. 8). At present, it has been over 2 years since the surgery, and no significant changes were observed during the follow-up period. A decrease in pain along the thoracolumbar spine is the only noticeable change.
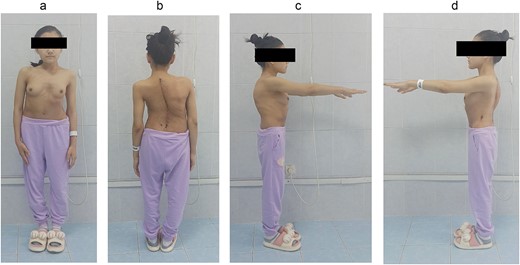
Postoperative patient’s appearance: (a) front, (b) back, (c) right side, and (d) left side.
Discussion
Congenital deformities of the spine should be operated on as early as possible. There are several variants of surgical treatment of patients with congenital deformities associated with diastematomyelia. A number of authors follow to a two-stage tactic during which the first stage is the removal of diastematomyelia and the second stage is the correction of scoliosis after 3–6 months [7, 8]. However, with this method, the total duration of the operation and the total amount of blood loss are much higher. Other authors are make choose one-stage correction in which both diastema resection and deformation correction are executed in one operation [9–11]. During this operation, the total time of the operation is shortened and the total amount of blood loss is decreased. The presence of modern equipment enables intraoperative monitoring in order to minimize possible complications. There are also studies that describe cases of correction of scoliosis without resection of the bone spur [12]. However, during our operation, there was a strong tension of the dura mater of the spinal cord in the process of the correction of deformation, which could lead to neurological complications with a preserved bone septum.
In conclusion, simultaneous tactics of surgical treatment may be the method of choice for congenital scoliosis associated with diastematomyelia, since the total length of the operation and the total volume of blood loss is significantly lower, and resection of the bone septum reduces the risk of neurological complications.
Author contributions
Each individual author contributed individually and significantly to the development of this work. The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. All authors have read and agree with the final manuscript of the article.
Conflict of interest statement
None declared.
Funding
Development and scientific justification of innovative technologies to improve the efficiency of diagnosis, treatment of injuries, consequences of injuries, diseases of the limbs, spine, and pelvis. BR11065157.



