-
PDF
- Split View
-
Views
-
Cite
Cite
Jiyeon Kang, Yeon Soo Kim, Ji-Ye Kim, Video-assisted thoracic surgery for an endobronchial ancient schwannoma obstructing the left main bronchus, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae140, https://doi.org/10.1093/jscr/rjae140
Close - Share Icon Share
Abstract
A schwannoma is a tumor that arises from the Schwann cells of the peripheral nerves. Primary pulmonary schwannomas are extremely rare, although they can occur anywhere in the body. Symptoms of endobronchial schwannoma vary depending upon the extent of bronchi blockage by the tumor. Schwannoma is a benign tumor. However, there is a risk of recurrence if a lesion that has developed extraluminal growth is incompletely resected. Here, a 76-year-old female patient presented with dyspnea and cough. An endobronchial tumor was identified originating from the left lower lobe bronchus and had collapsed the left lower lobe and grown to block most of the left main bronchus. Video-assisted thoracic surgery was performed to resect the left lower lobe. The tumor was diagnosed as an ancient schwannoma.
Introduction
Schwannomas are benign nerve sheath tumors that originate from Schwann cells and arise from the peripheral, spinal, or cranial nerves but not the optic or olfactory nerves. These tumors can occur anywhere else in the body. However, they are most common in the head, neck, and flexor surfaces of the upper and lower extremities [1]. Endobronchial schwannomas are rare. Although they have been reported, their exact frequency is unknown [2]. This is a late-presenting tumor, and some patients may be asymptomatic at presentation. Here, we present a case report of an endobronchial ancient schwannoma in the proximal part of the left lower lobe bronchus with obstruction of the left main bronchus. Complete resection was performed by thoracoscopic surgery.
Case report
A 76-year-old female patient presented to the hospital with dyspnea and coughing. A chest X-ray (Fig. 1a) revealed a possible tumor in the left main bronchus and atelectasis of the left lower lobe. A chest computed tomography scan confirmed an endobronchial tumor obstructing the left lower lobe bronchus that had grown toward the main bronchus to the point of near complete obstruction. A malignant tumor in the endobronchial region was suspected (Fig. 1b and c). Bronchoscopy was performed and revealed an endobronchial tumor with a smooth surface that obstructed most of the left main bronchus (Fig. 2). Blood vessels were visible on the tumor surface. The tumor did not appear amenable to endobronchial treatment or resection. The results of bronchoscopy suggested a benign tumor, although malignant disease could not be ruled out. Surgery was chosen for treatment.
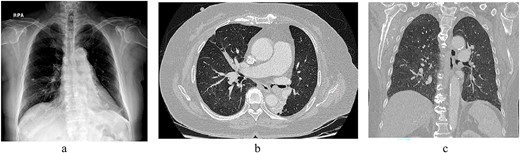
(a) Chest radiogram shows a possible tumor in the left main bronchus and atelectasis of the left lower lobe. (b) A chest computed tomography scan confirmed an endobronchial tumor obstructing the left lower lobe bronchus that was growing toward and nearly completely blocked the main bronchus. (c) Coronal view.
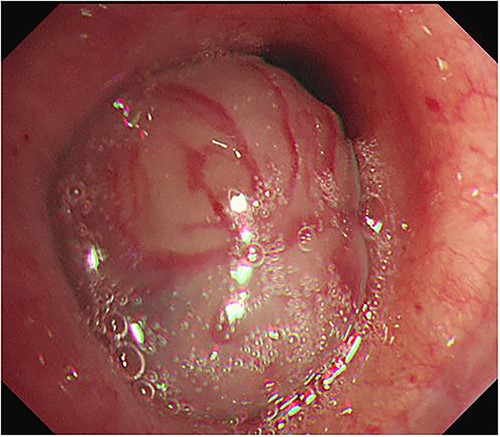
Bronchoscopy was performed and revealed an endobronchial tumor with a smooth surface that was obstructing most of the left main bronchus.
Video-assisted thoracoscopic surgery was used to perform a resection of the left lower lobe. The surgical procedure was carried out through a 4-cm surgical incision at the mid-axillary line of the fifth intercostal space, a 3-cm surgical incision at the mid-axillary line of the seventh intercostal space, and a 5-mm trocar incision at the midline and posterior axillary line of the sixth intercostal space. A 5-mm thoracoscope with a 30-degree view was used to perform the procedure. The left lower lobe bronchus was gradually resected after being incised. The tumor, which measured 1.8 × 0.8 cm, had grown a thin stalk attached to the left lower lobe bronchus. No invasion of the tumor into the surrounding tissue was observed (Fig. 3). The lower lobe bronchial stump was repaired with interrupted suture absorbable monofilament sutures. Pericardial fat was wrapped around the suture area. The postoperative course was uneventful, and the patient was discharged 9 days post-operation.
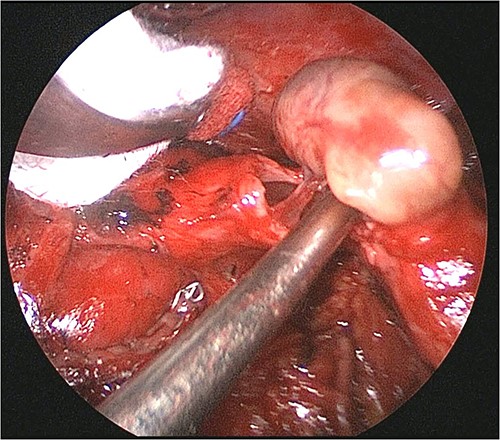
Operative findings. The tumor, which measured 1.8 × 0.8 cm, had a thin stalk attached to the left lower lobe bronchus. No invasion of the tumor into the surrounding tissue was observed.
The postoperative pathology revealed spindle cells with areas of hypercellular Antoni A and hypocellular Antoni B. The tumor also exhibited occasional cystic changes, hemosiderin pigments, and diffuse lymphocytic infiltration (Fig. 4a). Immunohistochemistry testing was positive for S-100 and SOX10, whereas the Ki67 LI result was <5% (Fig. 4b–d). These histological and immunohistochemical features were consistent with an ancient schwannoma.
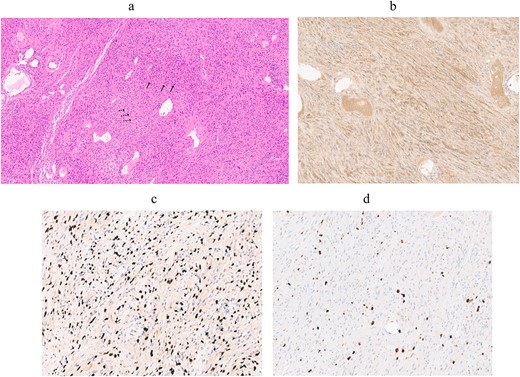
Pathological images. (a) On higher power (×20, objective), the tumor was composed of spindle cells with areas of hypercellular Antoni A (arrows) and hypocellular Antoni B (dotted line arrows). The tumor also had occasional cystic changes, hemosiderin pigments, and diffuse lymphocytic infiltration, all characteristics of an ancient schwannoma. (b, c) Immunohistochemical staining results showed uniform intensity for S-100 protein and SOX10. (d) The Ki67 LI staining was positive in <5% of cells.
Discussion
Neurogenic tumors comprise 15%–25% of all primary mediastinal tumors. Intrathoracic neurogenic tumors are found almost exclusively in the posterior mediastinum [3]. Primary pulmonary tumors of neurogenic origin are extremely rare. Roviaro et al. [4] reported that, among 1664 patients with pulmonary neoplasms, four cases (0.2%) were primary pulmonary neurogenic tumors, and one of these cases was malignant.
Pulmonary schwannomas can occur in any part of the respiratory tract, including the trachea, bronchus bronchioles, and alveoli [2]. They often progress into both intraluminal and extraluminal spaces. Schwannomas are slow-growing tumors that are usually asymptomatic and discovered incidentally on radiographs. Symptoms depend upon the location and size of the tumor and occur when it becomes large enough to block the bronchial tubes. Symptoms are nonspecific and include dry or productive cough, fever, hemoptysis, dyspnea, and postobstructive pneumonia [5].
Ancient schwannoma is a degenerative type with marked nuclear atypia. This tumor usually develops when a large tumor has been present for a long time. Degenerative changes include cyst formation, calcification, hemorrhage, and hyalinization. Tumors are typically infiltrated by numerous siderophages and histiocytes. The Schwann cell nuclei are large, hyperchromatic, and often multi-lobulated, but there are no mitotic figures. The nuclear atypia might be dismissed as a kind of degenerative change [6].
The choice of treatment for endobronchial schwannomas is complex. If the lesion occurs in the trachea or proximal bronchus, it may be visible by bronchofiberoscopy. There are types where the lesions grow into intraluminal and extraluminal spaces. In this case, even if endoscopic resection of intraluminal lesions is performed, recurrence may occur because of extraluminal progression. Half of intraluminal schwannomas have nonapparent extraluminal lesions, and incomplete resection of the lesion can lead to local recurrence. Nevertheless, presumably because of its slow-growing nature, many years may pass before onset of recurrence [2].
In this case, a tumor originating in the left lower lobe bronchus almost completely blocked the left main bronchus, and resection using a bronchoscope was expected to be difficult, so surgical treatment was chosen. Although the tumor was protruding into and blocking the left main bronchus, it was protruding from the left lower lobe bronchus. Therefore, the left lower lobe bronchus, rather than the main bronchus, was selected for resection. An incision was made, leaving the proximal part of the lower lobe bronchus for stump suturing. The tumor stalk was identified during resection of the left lower lobe bronchus. The tumor was completely resected without leaving any residue. Video-assisted thoracoscopic surgery for lobectomy can help to reduce the pain associated with a small incision size and can be performed without intercostal spread to improve the quality of life [7]. Our patient had an uneventful postoperative recovery.
Conflict of interest statement
None declared.
Funding
None declared.



