-
PDF
- Split View
-
Views
-
Cite
Cite
Hanan Tally, Moatasem Ali Hussein Al-janabi, Heba AlDwairy, Zuheir Al-Shehabi, Mostafa Ibrahim, Low-grade fibromyxoid sarcoma in laryngopharynx: the first case report in the literature, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae141, https://doi.org/10.1093/jscr/rjae141
Close - Share Icon Share
Abstract
Low-grade fibromyxoid sarcoma is a rare mesenchymal neoplasm with distinctive histopathological features. Although it typically arises in the deep soft tissues of the trunk and extremities, its occurrence in the head and neck region is exceedingly rare. We present the first documented case of low-grade fibromyxoid sarcoma in the laryngopharynx, expanding the spectrum of this rare tumor’s anatomical localization. The clinical, radiological, and histopathological features of this unique case are discussed, highlighting the diagnostic challenges and therapeutic considerations associated with this uncommon presentation.
Introduction
Low-grade fibromyxoid sarcoma (LGFMS) is a rare subtype of fibrosarcoma that was first described by Evans in 1987 [1]. It is characterized by a deceptively benign histological appearance with a predilection for deep soft tissues, typically involving the trunk and extremities [1, 2]. The tumor is known for its slow growth, indolent behavior, and a tendency for local recurrence [3]. However, its occurrence in the head and neck region is extremely rare, with limited cases reported in the literature [4].
Case presentation
A 63-year-old male presented with a 1-year history of dysphonia, hoarseness, choking, progressive dysphagia, and a sensation of throat obstruction. The patient, a smoker, denied cough and weight loss. Family history was unremarkable. Physical examination revealed no specific features, and there was no evidence of lymphadenopathy or distant metastasis. The strobolaryngoscopy was performed and a mass above the left vocal cord was identified (Fig. 1) (Video S1). The mass was completely resected using micro scissors under general anesthesia, with visualization using a microscope attached to the laryngoscope, and was subjected to pathologic examination. A gross examination of the resected mass revealed multiple fragments measuring 7 cm in maximum diameter (Fig. 2). Microscopically, there was diffuse and nodular proliferation of bland fusiform or stellate neoplastic cells in a myxoid stroma (Fig. 3A). The fibrotic areas are more cellular but the cells themselves appear similar to those in the myxoid areas (Fig. 3B). Tumor cells have small hyperchromatic nuclei (Fig. 3C and D). Mitotic figures are rare. In immunohistochemistry, cytokeratin is negative (Fig. 4A). Ki67 rate is very low (Fig. 4B and C). Tumor cells show positivity to vimentin (Fig. 4D). The diagnosis of LGFMS was made. After a follow-up period of 6 months, the patient had no signs of tumor recurrence or metastases, as confirmed by a computed tomography (CT) scan (Fig. 5).

Strobolaryngoscopy image shows the mass above the left vocal cord.

The gross image of the mass shows multiple fragments, all measuring 7 cm.
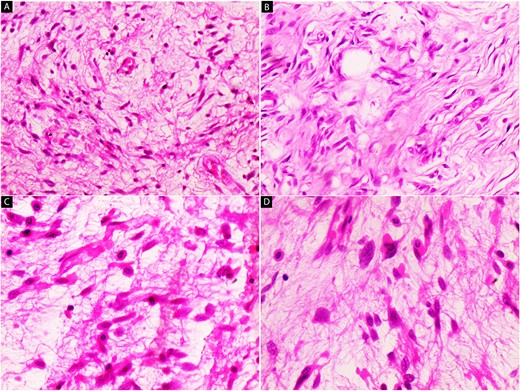
Hematoxylin and eosin stain (A–D); microscopic images of mass; (A) the low-power magnification shows diffuse and nodular proliferation of bland fusiform or stellate neoplastic cells in a myxoid stroma (40×); (B) the fibrotic areas are more cellular but the cells themselves appear similar to those in the myxoid areas (100×); (C and D) Bland fusiform or stellate neoplastic cells have small hyperchromatic nuclei (200× and 400×).
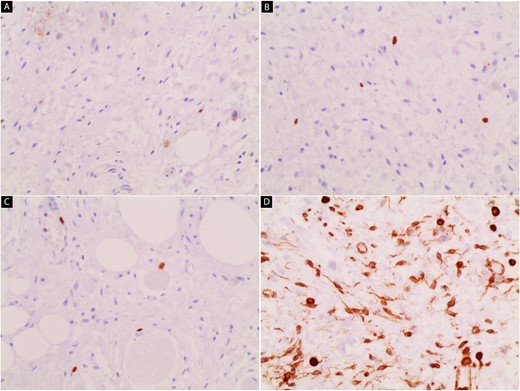
Immunohistochemical stain image; (A) cytokeratin is negative; (B and C) the ki67 rate is very low; (D) tumor cells show positivity to vimentin.
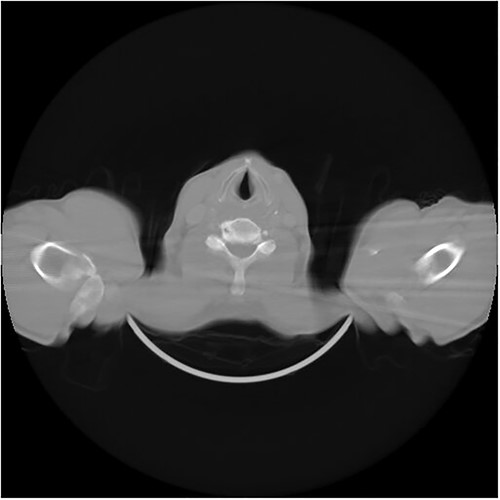
CT scan of the neck and throat image shows no signs of tumor recurrence or metastases.
Discussion
LGFMS is a distinctive entity within the spectrum of fibrosarcomas [1, 3]. Although it most commonly arises in the trunk and extremities, it has been reported in various anatomical sites, including the head and neck [4, 5]. The rarity of LGFMS in the laryngopharynx poses diagnostic challenges, as its clinical presentation and radiological features may mimic other more common neoplasms in this region [6]. Histopathologically, LGFMS is characterized by a proliferation of bland spindle cells arranged in a whorled pattern, embedded in a myxoid or fibrous stroma [2, 5]. The tumor’s deceptive histology can lead to misdiagnosis, with clinicians and pathologists often considering benign lesions or low-grade malignancies in the differential diagnosis [6]. Immunohistochemical analysis plays a crucial role in confirming the diagnosis of LGFMS, where most tumor cells were strongly positive for vimentin [2]. In this case, the immunohistochemical profile supported the diagnosis, ensuring accurate identification of this rare tumor in the laryngopharynx. The management of LGFMS involves complete surgical excision, as these tumors have a propensity for local recurrence [7, 8]. The surgical approach may vary depending on the tumor location and extent [8, 9]. In our case, a transoral excision was performed, aiming for complete removal while preserving laryngeal function. Postoperative surveillance with regular imaging studies is crucial to monitor for recurrence, given the tumor’s potential for delayed relapse [7, 9].
Conclusion
This case report presents the first documented occurrence of LGFMS in the laryngopharynx, expanding our understanding of the anatomical distribution of this rare tumor. The clinical, radiological, and histopathological features of this case underscore the importance of considering LGFMS in the differential diagnosis of laryngopharyngeal masses, despite its rarity in this region. Surgical excision remains the mainstay of treatment, and long-term surveillance is essential to monitor for potential recurrence. This case report contributes to the existing literature on LGFMS, providing valuable insights into its clinical behavior and management in an uncommon anatomical site.
Conflict of interest statement
None declared.
Consent
Written consent was obtained.
Guarantor
Moatasem Hussein Al-janabi.



