-
PDF
- Split View
-
Views
-
Cite
Cite
Max Frenkel, Timothy Guenther, Joshua Hermsen, Kelly Collins, Joshua Mezrich, David Al-Adra, Yu Xia, Primary inferior vena cava synovial sarcoma treated with caval replacement during cardiopulmonary bypass and ante situm liver perfusion, Journal of Surgical Case Reports, Volume 2024, Issue 12, December 2024, rjae760, https://doi.org/10.1093/jscr/rjae760
Close - Share Icon Share
Abstract
Primary inferior vena cava (IVC) tumors are rare. Most are leiomyosarcomas. The prognosis is poor with those involving and superior to the hepatic veins faring worse than those isolated within the retrohepatic cava. Tumors with superior extension were historically considered unresectable, though there are mounting reports of multicavity resections. We present an exceedingly rare case of a primary IVC synovial sarcoma treated with caval replacement to the right atrium (without hypothermic circulatory arrest) and hepatic vein reconstruction with autologous pericardium during ante situm liver perfusion. We highlight the value of multidisciplinary consideration for extensive primary caval tumors.
Introduction
Primary inferior vena cava (IVC) tumors are rare. Most are leiomyosarcomas (LMSs) and there are only six reported cases of primary IVC synovial sarcomas. The prognosis is poor with those involving and superior to the hepatic veins faring worse than those isolated to the retrohepatic cava. Extension into the right atrium historically precluded resection, but there mounting examples of multicavity resections.
Case description
A 36-year-old male with no significant medical history presented with a 10-day history of fatigue, abdominal bloating, bilateral lower extremity edema, and 20 lbs weight gain. Computed tomography (CT) scan of his abdomen revealed a 5-cm lobulated mass within the infra- and suprahepatic IVC extending into the right atrium. Magnetic resonance imaging (MRI) showed that the mass likely originated from the suprahepatic IVC and extended into both the infrahepatic IVC and right atrium (Fig. 1). A transfemoral biopsy diagnosed a poorly differentiated, monophasic synovial sarcoma. He was medically managed and discharged on hospital Day 4. An outpatient positron emission tomography CT failed to show evidence of metastatic disease. The case was discussed in a multidisciplinary conference, and the patient was thought to be a good surgical candidate.
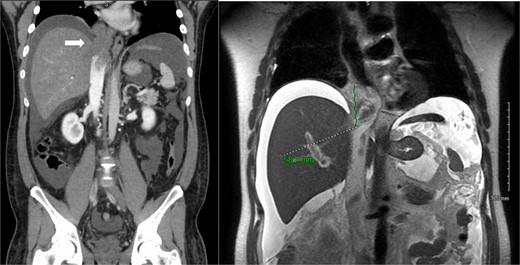
Primary IVC synovial sarcoma extending from the retrohepatic cava into the right atrium. Left: coronal slice of abdominal CT scan with IV contrast showing occlusive intravascular lesion (white arrow). Right: coronal abdominal MRI T2 slice demonstrating 5.8 cm enhancing intravascular lesion.
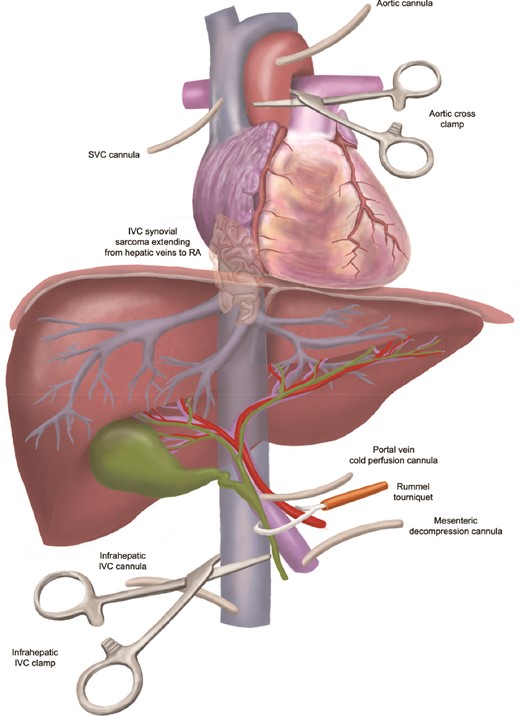
Three weeks after the initial presentation, the patient underwent caval resection and replacement with hepatic vein reconstruction. A thoraco-laparotomy was performed, and the transplant surgery team prepared for IVC resection and ante situm perfusion. The tumor and adjacent structures that it was invading were removed. The contents of the porta hepatis were dissected and encircled for a Pringle maneuver. Venous cannulae were placed in the infrahepatic IVC and the portal vein for complete vascular exclusion of the liver and to decompress the mesentery.
Meanwhile, the cardiac team procured pericardium for eventual hepatic vein reconstruction and placed the patient on cardiopulmonary bypass. The aorta and superior vena cava (SVC) were cannulated, the aorta was cross-clamped, and the heart was arrested with anterograde cardioplegia. The infrahepatic cava was clamped, the Pringle was applied, and the right atrium was opened. Cold preservation solution was delivered to the liver via the portal vein (Fig. 2). The atriotomy was extended down the IVC, the IVC was transected just inferior to the cavoatrial junction, the right atrial tumor mass was removed, and the atriotomy was repaired primarily. The liver was packed with ice and retracted into the ante situm position (rotated to expose the hepatic veins and IVC anteriorly). The hepatic veins were dissected and incised, and the tumor was removed.
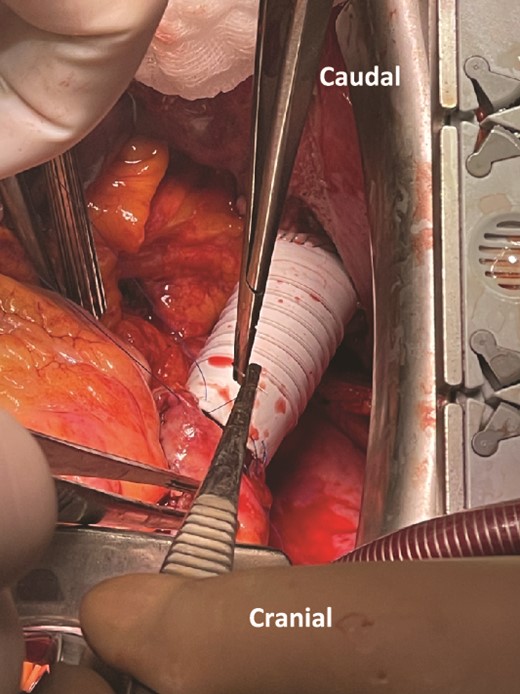
The IVC was replaced with a 2-cm diameter PTFE graft, and the hepatic veins were reconstructed. The right hepatic vein was anastomosed to the graft in an end-to-side fashion while the left and middle hepatic veins were augmented with autologous pericardium before performing an end-to-side anastomosis. The liver was then replaced in its anatomic position, and the superior aspect of the graft was anastomosed to the right atrium (Fig. 3). The liver was flushed with blood by removing all inflow clamps. The inferior aspect of the graft was clamped again thereby establishing portal venous return to the right heart through the reconstructed hepatic veins. Finally, the infrahepatic cava was anastomosed to the inferior aspect of the graft, and the infrahepatic caval clamp was removed to de-air the graft before the anastomosis was completed. The patient was weaned from bypass, and his immediate postoperative course was uncomplicated (Clavien-Dindo grade I). He was discharged on post-operative Day 10.
One of four sample margins was positive for multifocal microscopic involvement (R1), so he underwent adjuvant radiation. The most recent chest CT scan at 7 months post-reconstruction demonstrated new likely lung metastases. He otherwise denies abdominal pain, bloating, or lower extremity edema suggesting preserved outflow.
Discussion
Primary venous sarcomas are rare. The most common subtype is LMS of the IVC. The largest existing dataset consists of only ~400 cases despite spanning over 6 decades [1]. Despite the data scarcity, there seems to be a female predominance, patients often present in the fifth decade of life, and surgical resection is rarely curative with a 5-year disease-free survival of only ~5%. Tumor location is an important prognostic variable; tumors confined to the retrohepatic cava may carry the best prognosis whereas those at the level of and superior to the hepatic veins (Vollmann’s type IV) portend the worst. Within type IV, a rare subset invades the right atrium. Of 377 IVC LMSs reported, only 19 (5%) extended into the right atrium. For the 315 cases with operative details, 11 (3.5%) used cardiopulmonary bypass, probably representing the set of tumors with right heart involvement. In a separate case series, only 2 of 22 patients with IVC-LMS had right heart involvement one of which underwent a resection under deep hypothermic circulatory arrest [2]. Because of the paucity of data, poor survival, and surgical challenges of type IV IVC sarcomas, these have been historically deemed inoperable or have required complicated approaches such as neo-adjuvant chemo-radiation for tumor debulking [3].
Even more rare are primary IVC synovial sarcomas with only six reported cases [4, 5]. Five were histologically biphasic and all were found in women. All six cases required resection, but only one demonstrated intracardiac extension for which excision was performed under deep hypothermic circulatory arrest. Our case is unique both because of the patient’s features and because of the surgery. First, this patient is a young male with monophasic type IV primary IVC sarcoma extending into the right atrium: exceptionally rare characteristics. Second, we performed complete macroscopic resection (without neoadjuvant therapy) and reconstructed the IVC and hepatic outflow while on cardiopulmonary bypass and the liver was protected with ante situm cold perfusion. While ante situm perfusion has been described for IVC tumors (whether primary or locally invasive), to our knowledge it has not been combined with cardiopulmonary bypass specifically to resect a type IV tumor that involves the right atrium. This approach avoids the many risks associated with deep hypothermic circulatory arrest. We suggest that many historically unresectable IVC tumors involving the hepatic veins and right heart may be operable with a multidisciplinary approach.
Acknowledgements
We would like to thank Ashley Doherty for her illustration of the anatomy.
Conflict of interest statement
None declared.
Funding
None declared.
Informed consent
Patient consent obtained.
References
Tong G-X, Goldblum JR, Qiu W, et al. Primary intravascular synovial sarcoma: a disease of young adult women? Report of a case diagnosed by aspiration biopsy and review of the literature.



