-
PDF
- Split View
-
Views
-
Cite
Cite
Hanan Qunibi, Mariam Thalji, Mutasem Sayyed Ahmad, Sulaiman Fakhouri, A rare case of tip appendicitis treated successfully with conservative management, Journal of Surgical Case Reports, Volume 2024, Issue 11, November 2024, rjae685, https://doi.org/10.1093/jscr/rjae685
Close - Share Icon Share
Abstract
Tip appendicitis is a rare and fatal complication after appendectomy. Diagnosing this condition requires a high level of suspicion due to its ambiguous and nonspecific symptoms. Radiological investigations such as ultrasound and computed tomography scans can aid in diagnosis. Early identification and treatment are of paramount importance for good patient outcomes. In most cases, Tip excision is the preferred treatment. However, antibiotics can also be a useful alternative. Conservative antibiotic treatment can be successful in certain situations, particularly when no fecaliths or perforation exists. Close monitoring is necessary to avoid the return of chronic appendicitis. We here introduce a case of a 47-year-old female patient who underwent an open appendectomy a year ago and is currently complaining of right lower quadrant abdominal pain. The patient was diagnosed with tip appendicitis. She was started on conservative antibiotic therapy and discharged home with good general conditions.
Introduction
Appendicitis is one of the most common abdominal surgical emergencies, which has an incidence rate of approximately 233 per 100 000 individuals [1–3]. Appendectomy is a commonly performed surgical procedure worldwide, and it is considered the definitive treatment of appendicitis [1, 4, 5]. Recurrent appendicitis is a rare complication after an appendectomy, occurring after 1 in 50 000 appendectomies [6]. The majority of the cases are caused by an inflammatory process involving the appendiceal stump. On the other hand, a very few numbers of cases result from inflammation in the retained appendiceal tip [5, 6]. Here, we present a case of a 47-year-old female patient who was found to have residual tip appendicitis diagnosed one year after the appendectomy and underwent successful medical management.
Case presentation
A 47-year-old female patient known case of hypertension and diabetes mellitus. Her past surgical history includes an open appendectomy for acute gangrenous appendicitis 1 year ago. During the initial appendectomy, the appendiceal root was ligated, but the appendix was not completely removed, and the tip of the appendix left due to severe inflammation and adhesions.
The patient presented recently to our ER complaining of peri-umbilical pain radiating to the right iliac fossa for one-month duration, with gradual onset, colicky in nature, associated with vomiting five times and diarrhea four times. The pain does not change with position or medications. The menstruation is regular, with normal amount, lasting for five days. The last menstrual period was five days before the recent presentation. The patient denied any history of fever or NSIAD use. There is no history of urinary frequency, dysuria, or hematuria. Gastrointestinal wise, she has no history of constipation, melena, or hematochezia,
Upon examination, the patient’s vital signs were stable, Temperature:36.8°C, BP:128/78 mmHg, and HR:82 beat/min. She looks well, active, and alert. She appeared mildly in pain. Abdominal exam showed a soft lax abdomen with generalized tenderness, mainly on the right lower fossa. Rebound pain and rovsing sign were positive. Otherwise, the patient is clinically normal.
Further investigations were done to confirm the diagnosis, CBC showed elevated WBC with left shifting, and C-reactive protein (CRP) was positive at 16 g/l. gynecological consulted to exclude any gynecological cause, the ultrasound was free. Urine analysis was done, and it was free. For that, with the history of initial appendectomy, subsequent abdomen, and pelvic computed tomography (CT) with contrast was performed. Findings represent inflammation of the distal part of the residual appendix associated with mucosal enhancement and mild surrounding fat stranding, confirming the diagnosis of recurrent tip appendicitis (Fig. 1).
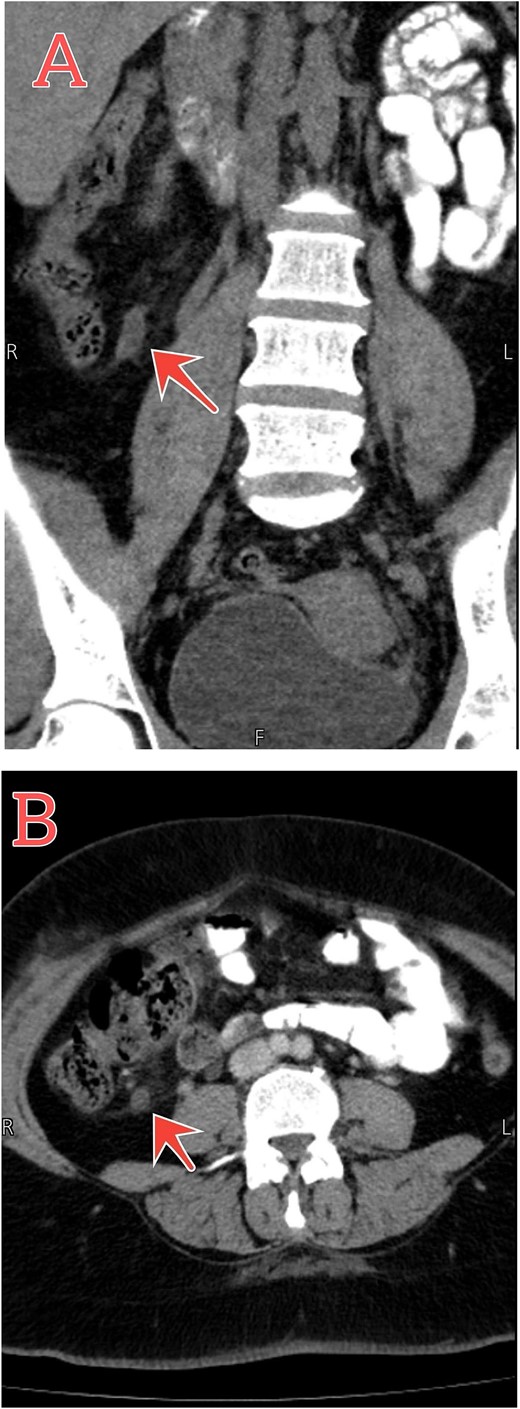
Abdomen–pelvic CT scan shows tip appendicitis. (A and B) Coronal and axial sections show the distal part of a blind-ended tubular structure measuring about 8 mm arising from the cecum (red arrows), associated with mucosal enhancement and mild surrounding fat stranding.
The patient was treated conservatively for two days by giving IV cefuroxime 1.5 mg three times per day, metronidazole 500 mg three times per day, pantoprazole 40 mg once daily, and acetaminophen 1 mg four times per day. Follow-up CT scan showed resolution of the condition (Fig. 2). She was discharged back home with good general conditions without complications.
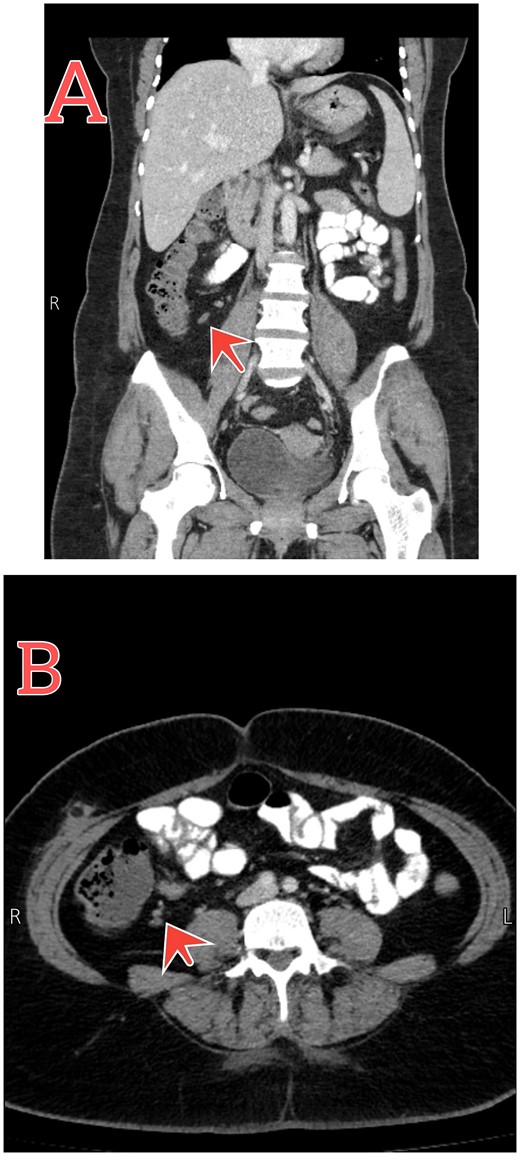
Follow-up abdomen–pelvic CT scan. (A and B) Coronal and axial sections show resolution of the inflammatory process postconservative management (red arrows).
Discussion
Appendicitis is a common surgical condition that is usually treated by resection of the inflamed appendix [7]. On the other hand, acute residual tip appendicitis is a rare condition, where a remnant of a partially removed appendix is inflamed postinitial appendectomy [8]. It is considered a late and under-reported complication post either open or laparoscopic appendectomy [7].
Patients with previous history of appendectomy may have a missed or late diagnosis of tip appendicitis causing serious complications like perforation. The presentation of acute residual tip appendicitis varies, and patients may present with atypical signs and symptoms and with either acute or subacute course [8]. The interval between the episodes differs from a few weeks to approximately 50 years after the first appendectomy [9]. In this case, the presentation of the residual appendiceal tip was one year postappendectomy. Residual tip appendicitis has a higher morbidity rate than the first presentation of appendicitis [8, 10].
The clinical diagnosis of residual tip appendicitis may be challenging considering the atypical presentation that may be introduced postappendectomy [7]. Besides the history and clinical examination, labs like CBC show a left shifting of PMNS, and CRP is usually elevated as in our case.
Abdominal ultrasound is the initial radiological investigation to confirm the diagnosis of acute appendicitis [7]. In the case of residual tip appendicitis, using this imaging may be difficult to confirm the diagnosis. However, as the ultrasound may cause incomplete visualization, CT usually is used to confirm the diagnosis.
The definitive management of most residual appendicitis is surgical via open operations with a high success rate as reported in many literatures. The laparoscopic approach is also used in some cases successfully. On the other hand, previous surgical history of appendectomy makes the adhesions difficult to lyse with laparoscopy, and this indicates the surgical treatment with laparotomy [8–10]. In this case, we followed the conservative management for two days by giving the patient iv cefuroxime 1.5 mg three times per day, metronidazole 500 mg three times per day, and pantoprazole 40 mg once daily. The medical treatment has been showed a good results and the patient discharged without any complications.
Conclusion
Recurrent tip appendicitis is a rare condition in the surgical field that faces diagnostic challenges. Therefore, even though it is rare, doctors should consider the possibility of recurrence of appendicitis in individuals who have undergone previous appendectomies and exhibit classic symptoms of appendicitis. Conservative treatment with antibiotics can be successful in certain cases, especially when no fecaliths or perforations.
Conflict of interest statement
There is no conflict of interest to declare.
Funding
The study did not receive any funding.
Consent
Written informed consent was obtained from the patient family for reporting this case and its associated images. The consent is available for review on request.
References
Lotfollahzadeh S, Lopez RA, Deppen JG.



