-
PDF
- Split View
-
Views
-
Cite
Cite
Paola Solis-Pazmino, Iván Hernandez, Erika Gordon, Estefania Clavijo, Estefania Alvarado, Eddy Lincango, Andrés Cedeño, Puestow surgery in a SPINK mutation chronic pancreatitis: a rare case report, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae614, https://doi.org/10.1093/jscr/rjae614
Close - Share Icon Share
Abstract
This case report highlights the clinical presentation and surgical management of a 27-year-old man with recurrent pancreatitis attributed to a homozygous SPINK1 (N34S) mutation. The patient, who experienced multiple hospital admissions, underwent extensive diagnostic evaluations, including imaging and genetic testing, confirming the hereditary nature of his condition. Despite unsuccessful endoscopic interventions, a laparoscopic Puestow procedure was performed, aiming to alleviate symptoms and improve pancreatic drainage. Postoperatively, the patient's recovery was successful, and he was discharged with supplemental pancreatic enzyme therapy. The differential diagnosis included autoimmune pancreatitis and non-hereditary chronic pancreatitis. This case underscores the challenges and considerations in the diagnosis and management of hereditary pancreatitis associated with SPINK1 mutations, emphasizing the role of surgical interventions for selected cases.
Introduction
SPINK1 (Serine Protease Inhibitor Kazal type 1) is a gene associated with hereditary pancreatitis. Mutations in the SPINK1 gene can produce a dysfunctional pancreatic secretory trypsin inhibitor (PSTI), leading to uncontrolled trypsin activity and subsequent inflammation and damage to the pancreas [1].
It is most common at a younger age. Hereditary pancreatitis linked to SPINK1 mutations presents with symptoms such as persistent abdominal pain, digestive issues, nausea, vomiting, and recurrent episodes of acute pancreatitis. Diagnosis includes clinical evaluation, imaging tests, blood tests for pancreatic enzyme levels, genetic testing for SPINK1 mutations, and possibly procedures like ERCP [2].
When conservative treatments are insufficient, and there is a localized area of the pancreas causing significant problems, a pancreatic surgery resection is performed [3]. The Puestow procedure, or lateral pancreaticojejunostomy, is a surgical technique used to treat chronic pancreatitis. A laparoscopic Puestow procedure involves creating an anastomosis between the pancreatic duct and the jejunum through small abdominal incisions, improving pancreatic juice drainage [4]. The minimally invasive approach offers benefits such as reduced postoperative pain and faster recovery.
This case report aims to present the clinical features and surgical management of a patient with recurrent pancreatitis due to SPINK1 mutation.
Case presentation
A 27-year-old man from recurrent pancreatitis. The severity of his symptoms resulted in fourteen hospital admissions. On his third admission, he had acute renal insufficiency and started hemodialysis. After two years, he underwent a renal transplantation. On his fifth admission, he had hyperthyroidism and he underwent a parathyroidectomy. He was otherwise well, with no comorbidities and no prior surgeries. There was no family history of pancreatic disease or any history of alcohol or drug use.
An abdominal ultrasound (Fig. 1), a computed tomography (Fig. 2) and a magnetic resonance cholangiopancreatography (MRCP) resonance showed diffuse dilation of the main pancreatic duct the duct of Santorini and the secondary ducts. Stones inside the main pancreatic duct in the head region, measuring approximately 1.1 cm. Reduction in the thickness of the pancreatic parenchyma, associated with small calcifications in between (Fig. 2).

Abdominal ultrasound shows a diffuse dilation of the main pancreatic duct.

Abdominal computed tomography shows a diffuse dilation of the main pancreatic duct and Santorini duct, as well as dilation of secondary ducts. There are stones in the main pancreatic duct in the head region. Also, there is a reduction in the thickness of the pancreatic parenchyma, associated with small intervening calcifications, possibly due to chronic pancreatitis.
Medical causes of pancreatitis, including metabolic disorders, were excluded after extensive investigations by the clinic team. Due to his young age and his several admissions, he was referred for genetic testing and counseling. He tested positive for the homozygous variant of the SPINK1 (N34S) mutation.
He underwent two endoscopic retrograde pancreatography. In the last- one, the pancreatic duct was cannulated, and an unsuccessful attempt to place a prosthesis due to pancreatic stenosis (Fig. 3).
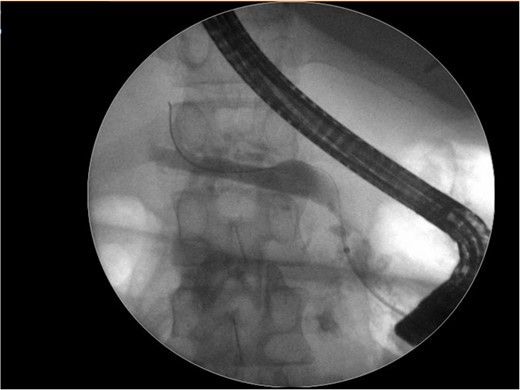
Endoscopic retrograde pancreatography shows an unsuccessfully cannulated pancreatic duct.
Given his symptomatic clinical course, he was referred to Digestive Surgery, to analyze a surgery option. The Puestow procedure was performed via a laparoscopic approach. The pancreatic body was exposed via the gastrocolic omentum. Localization of the PD was challenging to identify due to atrophic and calcified pancreas.
The pancreatic body was exposed via the gastrocolic omentum. The main pancreatic duct was identified with the use of intraoperative ultrasound and the duct opened longitudinally. The jejunum was transected 20 cm from the duodenojejunal flexure, and a 40 cm Roux loop was brought up in a retrocolic fashion. A single-layer side-to-side pancreatojejunostomy was done using 3–0 mersilk from the pancreatic head to the tail.
The patient’s postoperative course was unremarkable. He was discharged on supplemental pancreatic enzyme therapy.
Differential diagnosis
The diagnosis of hereditary pancreatitis associated with SPINK1 mutations involves ruling out other conditions that may present with similar symptoms. The conditions that might be considered in the differential diagnosis are Autoimmune Pancreatitis, and non-hereditary chronic pancreatitis (long-term alcohol use). Hyperparathyroidism (our patient underwent parathyroidectomy), Biliary Gallstones (our patient had cholecystectomy), and Cystic Fibrosis (genetic test was negative).
Discussion
SPINK hereditary pancreatitis is a rare form of chronic pancreatitis (less than 1% of carriers), the N34S is the most common variant. The prevalence of hereditary pancreatitis may vary across different geographic regions and ethnic groups [5].
Hereditary pancreatitis, including cases associated with SPINK1 mutations, may lead to chronic inflammation of the pancreas, increasing the risk of complications such as pancreatic insufficiency, diabetes, and an elevated risk of pancreatic cancer compared to the general population [6].
The decision to undergo a laparoscopic Puestow procedure is based on the severity of chronic pancreatitis symptoms and the failure of conservative management [7]. The laparoscopic technique offers several advantages over traditional open surgery. The use of small incisions reduces postoperative pain, shortens hospital stays, and speeds up recovery. The primary goal of the procedure is to enhance the drainage of pancreatic secretions. By creating an anastomosis between the pancreatic duct and the jejunum, the surgeon aims to reduce pressure within the pancreatic duct, alleviating symptoms associated with chronic pancreatitis, such as pain and malabsorption [8].
Following the laparoscopic Puestow procedure, patients require careful postoperative monitoring. Pain management, dietary adjustments, and close observation of potential complications are essential aspects of the recovery process [9].
Patient perspective
Living with hereditary pancreatitis, especially when associated with genetic mutations like SPINK1, can have a significant psychosocial impact. Individuals may face challenges related to chronic pain, dietary restrictions, and the risk of complications. Support from healthcare professionals, genetic counselors, and patient support groups can be valuable in addressing these aspects.
Conflict of interest statement
The authors declare that there is no conflict of interest.
Funding
The authors declare that there is no funding support for this manuscript.
Author contributions
Paola Solis-Pazmino and Andrés Cedeño conceived and designed the work. Paola Solis-Pazmino and Iván Hernandez wrote the manuscript. Erika Gordon and Estefania Clavijo: data collection. Paola Solis-Pazmino, Estefania Alvarado, and Andrés Cedeño: corrections and final article revision.
Ethical standards
All procedures followed were by the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from the patient to be included in the study.



