-
PDF
- Split View
-
Views
-
Cite
Cite
Koki Kawakami, Yoshihiro Moriwaki, Jun Otani, A case of idiopathic superior lumbar hernia repaired using a transabdominal laparoscopic approach, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae608, https://doi.org/10.1093/jscr/rjae608
Close - Share Icon Share
Abstract
The patient is a 78-year-old woman who presented to our hospital with left lumbar back pain as her chief complaint. She was diagnosed with superior lumbar hernia. There was no history of abdominal or lumbar surgery, or trauma, so the condition was considered idiopathic. Mesh was placed laparoscopically to repair the hernia. She was discharged on the second postoperative day. One year has passed since the surgery, and there has been no recurrence of the hernia, nor have there been any complications such as neuropathic pain. Superior lumbar hernia is a type of abdominal wall hernia that protrudes through the superior lumbar triangle and is a relatively rare condition. Due to the lack of an established standard surgical procedure, various surgical techniques have been employed depending on the facility. Laparoscopic surgery was considered a minimally invasive and reliable method for hernia repair, providing good visualization in cases without intra-abdominal adhesions.
Introduction
A superior lumbar hernia is a type of abdominal wall hernia that protrudes through the superior lumbar triangle and is relatively rare [1]. Due to the low number of cases and the lack of an established standard surgical procedure, various techniques have been used for treatment depending on the facility. Recently, there has been an increase in tension-free repair using mesh [2]. In this report, we present a case of idiopathic superior lumbar hernia treated with laparoscopic hernia repair using a mesh with an anti-adhesion barrier.
Case presentation
A 78-year-old female visited the orthopedic department of our hospital due to the left lumbar back pain and was referred to our department with a suspected idiopathic left superior lumbar hernia. She had a history of cerebral infarction, dyslipidemia, but no history of abdominal or lumbar surgery and history of trauma.
Swelling and tenderness were observed in the left lumbar back area. Abdominal contrast-enhanced CT showed the herniation of the retroperitoneal fat tissue into the abdominal wall was observed dorsally to the left kidney (Fig. 1). Surgery was performed because the pain persisted and there was a possibility of organ incarceration in the future. We used the laparoscopic system to perform the operation. The patient was positioned in the right lateral decubitus position under general anesthesia. A camera was inserted at the umbilicus, and 5 mm ports were placed in the epigastric region and left lower abdomen. The omentum and descending colon were adhered to the abdominal wall and were dissected. The descending colon was dissected laterally along the white line, and the dorsal side of the Gerota’s fascia was dissected. A 3 cm × 2 cm hernia orifice, bordered by the 12th rib lower edge, internal oblique muscle, serratus posterior inferior muscle, and quadratus lumborum muscle, was identified (Fig. 2). Part of the fatty tissue, including Gerota's fascia, was herniated, and it was resected as much as possible. A BARD Ventralight ST 10.2 × 15.2 cm mesh was placed, and it was fixed to the ribs and muscles using the double crown method with AbsorbaTack (Fig. 3). The operative time was 109 minute, with little blood loss. The patient discharged on postoperative Day 2 without postoperative complications. One year has passed since the surgery, and there have been no recurrence of the hernia, neuropathic pain.
Abdominal contrast-enhanced CT showed the herniation of the retroperitoneal fat tissue into the abdominal wall was observed dorsally to the left kidney(arrow).
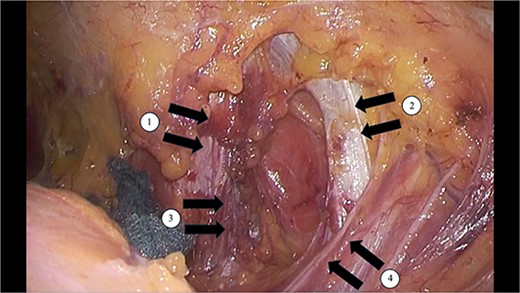
A 3 cm × 2 cm hernia orifice, bordered by the ①12th rib lower edge, ②internal oblique muscle, ③serratus posterior inferior muscle, and ④quadratus lumborum muscle, was identified.
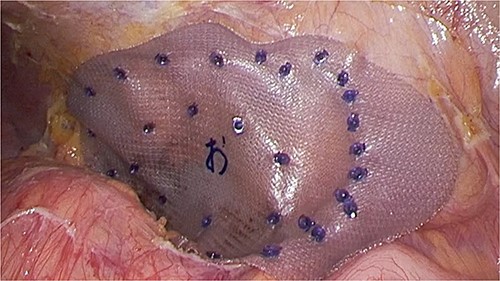
A BARD Ventralight ST 10.2 × 15.2 cm mesh was placed, and it was fixed to the ribs and muscles using the double crown method with AbsorbaTack.
Discussion
A superior lumbar hernia is a type of abdominal wall hernia that occurs in the superior lumbar triangle, and it is a relatively rare condition. The superior lumbar hernia arises in an anatomically weak area bordered by the lower edge of the 12th rib, the internal oblique muscle, the serratus posterior inferior muscle, and the quadratus lumborum muscle, with its surface covered by the latissimus dorsi muscle [3]. These hernias can be congenital or acquired. Approximately 10% are congenital, typically caused by underdevelopment of the lumbar muscles, the 12th rib, the spine, or the iliac bone [3, 4]. Acquired hernias can be classified as either idiopathic or traumatic, with the majority being idiopathic, often triggered by age-related spinal changes, muscle weakness, obesity, or increased abdominal pressure due to coughing. Traumatic hernias may occur following events such as traffic accidents, kidney removal, or iliac bone harvesting. In the present case, there was no history of trauma or surgery, and no musculoskeletal abnormalities were detected, leading to a diagnosis of an acquired idiopathic hernia due to aging.
Observation often leads to further widening of the hernia orifice and weakening of the surrounding tissues, making repair more difficult. Therefore, surgical repair is considered the first-line treatment [2]. Traditionally, the Petit operation, which involves direct suturing of the abdominal oblique and dorsal muscle groups, has been performed. In cases where the hernia orifice is large or the surrounding tissues are weak, muscle flap transplantation using the gluteus maximus or latissimus dorsi has also been reported. However, due to the rarity of cases, a standard surgical procedure has not been established, and various modifications are made depending on the institution.
In recent years, with the development and widespread use of laparoscopic surgery, there has been an increase in reports of tension-free laparoscopic repair [2, 5, 6]. The advantages of this approach include the ability to visualize the hernia orifice directly, allowing for appropriate mesh placement with proper margins, and the ability to identify nerve pathways to avoid postoperative neuropathic pain. However, the disadvantages include the difficulty of obtaining a clear view in cases with adhesions from previous surgeries, as well as the risk of organ injury.
Among abdominal wall hernias, laparoscopic repair of lumbar hernias is considered particularly challenging. However, the recurrence rate is reported to be 2.9% for laparoscopic surgery compared with 15% for open surgery, suggesting that laparoscopic surgery is superior in terms of recurrence rate [7]. Additionally, laparoscopic surgery is associated with less postoperative pain and shorter hospitalization and recovery times [8]. In this case, since there was no history of surgery, we opted for a laparoscopic approach. The 12th rib lower edge, internal oblique muscle, serratus posterior inferior muscle, and quadratus lumborum muscle, which served as landmarks, were identified, and the superior lumbar hernia was repaired using a mesh with an anti-adhesion barrier. Laparoscopic hernia repair was considered a procedure that allows for secure mesh fixation while maintaining a good surgical view, contributing to reduced postoperative pain and shorter hospital stays.
In conclusion, laparoscopic hernia repair was performed for idiopathic superior lumbar hernia. Laparoscopic surgery was considered a minimally invasive and reliable method for hernia repair, as it provides a clear surgical view in cases without intra-abdominal adhesions. Establishing a treatment method through the accumulation of more cases is desired.
Acknowledgements
I would like to thank Y Moriwaki for useful discussions. I am grateful to J Otani for carefully proofreading the manuscript.
Conflict of interest statement
None declared.
Funding
None declared.
Informed consent statement
Written informed consent was obtained from the patient for the publication of this case report and accompanying images.



