-
PDF
- Split View
-
Views
-
Cite
Cite
Sachiko Kimizuka, Hiroyuki Yamada, Koji Kawaguchi, Toshikatsu Horiuchi, Akira Takeda, Yoshiki Hamada, Bilateral chylothorax following left neck dissection and literature review, Journal of Surgical Case Reports, Volume 2024, Issue 1, January 2024, rjad723, https://doi.org/10.1093/jscr/rjad723
Close - Share Icon Share
Abstract
Chylothorax without chyle cervical leakage after neck dissection it is extremely rare. We report a case of bilateral chylothorax without chyle cervical leakage after left neck dissection, wherein partial left upper jaw resection and left radical neck dissection were performed in a 46-year-old woman who was diagnosed with left upper gingival cancer. The thoracic duct was ligated and cut during surgery and, although no obvious leakage of lymph was observed, dyspnea and cough reflex during deep inhalation were observed from the third postoperative day. Approximately 600 mL of yellowish-white pleural effusion was aspirated during bilateral thoracentesis, and chylothorax was diagnosed based on clinical findings and biochemical analysis results. The patient was put on a low-fat diet on the fourth postoperative day. Pleural effusion disappeared on imaging examination 16 days after thoracentesis.
Introduction
Chylothorax is an accumulation of chyle, a milky fluid usually of lymphatic origin, in the pleural cavity. Chylothorax causes cardiovascular abnormality, respiratory insufficiency, undernutrition, electrolyte abnormality, and immunodeficiency due to copious chyle exudation to the thoracic cavity [1] and prompt management is required in these cases.
Chylothorax is a frequent complication caused by injury to the thoracic duct during thoracotomy. However, the incidence of chylothorax with chylous fistula following neck dissection is reportedly 0.2% [2]. Moreover, chylothorax without chylous fistula is rare, associated with head and neck cancer. The diagnosis of chylothorax without chylous fistula is relatively difficult because of its rarity and the lack of visible findings such as neck swelling or white fluid in the drain tube in the early postoperative stage.
Herein, we report a rare case of bilateral chylothorax, without chylous fistula, following neck dissection for the treatment of upper gingival cancer, which was resolved with conservative treatment.
Case report
A 46-year-old woman was referred to the Department of Oral and Maxillofacial Surgery at Tsurumi University Dental Hospital in July 2014 for diagnosis and treatment of swelling in left upper molar region. She reported mobility of the second molar for approximately 2 years. Her past medical and family histories were unremarkable. An extroverted mass with an induration measuring 2.9 cm in diameter was found in the left maxilla upon physical examination. No neuroparalysis or cervical lymphoadenopathy was seen.
Partial maxillary resection was performed under general anesthesia in August 2014, based on a clinical diagnosis of upper gingival cancer (cT2N0M0). The defect was closed with a buccal fat pad.
The postoperative course was uneventful; however, rapid enlargement of left cervical lymph nodes was observed at 1 month after surgery. Contrast-enhanced CT showed enlarged left cervical lymph nodes with ring enhancement, and a diagnosis of secondary cervical lymph node metastasis was made (Fig. 1). Left radical neck dissection was performed under general anesthesia in October 2014, and a thick thoracic duct was found in the supraclavicular fossa during surgery. There was no leakage of lymph after ligation and cutting of the thoracic duct (Fig. 2), and the operation was completed following placement of three suction drains in the left neck.
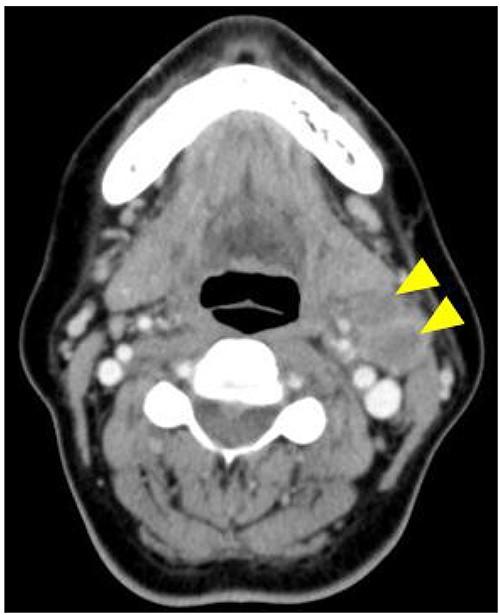
Contrast-enhanced CT is showing enlarged left cervical lymph nodes with ring enhancement (arrowheads).
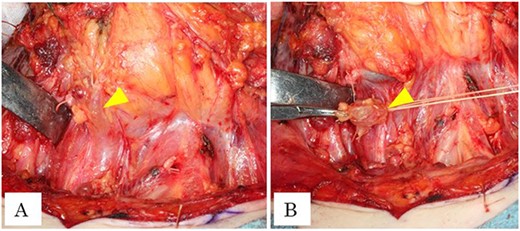
(A) Intraoperative photograph is showing dilation of thoracic duct (arrowhead). (B) Intraoperative photograph is showing ligation of thoracic duct (arrowhead).
The patient was started on a diet the first day after surgery. On the third day postoperative, she complained of respiratory distress in a supine position, and cough reflex was observed during deep inhalation. Chest X-rays and CT showed pleural effusion in both lower lung fields (Fig. 3), and chylothorax was suspected based on the intraoperative and postoperative clinical findings. Approximately 600 mL of yellowish-white pleural fluid was aspirated during bilateral thoracic puncture. Furthermore, no swelling of the neck was observed, and the contents of the neck drain were serous and had a concentration of 15 mg/dL of triglyceride, which was within the normal range. Therefore, no evidence of chyle leakage was observed in the neck. On the other hand, the triglyceride concentration of the pleural effusion was 705 mg/dL, which was significantly higher than that of the standard value. The patient was diagnosed with bilateral chylothorax without cervical chyle, according to the above results, but pleural effusion subsequently improved and respiratory distress disappeared. A low-fat diet was started on the fourth day after surgery, and all neck drains were removed on the eighth day postoperative. The pleural effusion on the chest radiograph disappeared 16 days after thoracentesis (Fig. 4), and postoperative chemoradiotherapy was performed since extra-nodal spread was observed in the left cervical lymph nodes (level II and III), determined through histopathology.
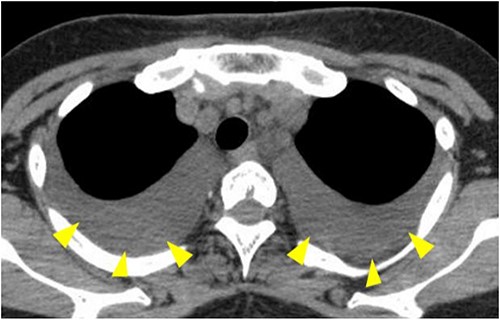
CT showing pleural effusion in both lower lung fields (arrowheads).
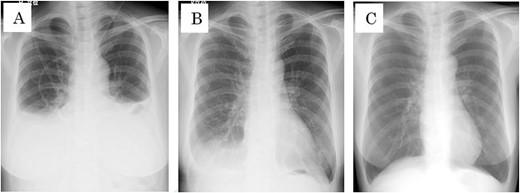
(A) Chest x-rays before bilateral thoracic puncture. (B) Chest X-ray 7 days after bilateral thoracic puncture. (C) Chest X-ray 16 days after bilateral thoracic puncture.
The postoperative course was uneventful, and there was no evidence of recurrence at follow-up examination 5 years and 6 months after surgery.
Discussion
Only 10 cases of chylothorax without chylous fistula were reported in the literature [3–10], associated with head and neck cancer (Table 1). The normal range of internal pressure for the thoracic duct is reported as 10–25 mmHg; however, the internal pressure can rise to 50 mmHg due to duct closure [11]. Bilaterally affected chylothorax is related to the anatomical pathway of the thoracic duct. The thoracic duct originates at the cisterna chyli in front of L1 and L2 and ascends along with abdominal aorta into the thoracic cavity. At the level of T4, and T5, it turns left and ascends along with esophagus to finally join the left vein angle [12]. Although lymphangiography or lymph scintigraphy was not performed to avoid complications in this case, the point of thoracic duct rupture was estimated approximately at the level of T4 and T5, or the upper stream where chyle can spread to the bilatelal thoracic cavity.
10 cases of chylothorax without chylous fistula associated with head and neck cancer.
| Case . | Year . | Author . | Primary . | Neck dissection . | Radiation . | Age/Sex . | Treatment . |
|---|---|---|---|---|---|---|---|
| 1 | 2001 | Al Sebein K et al. [3] | Larynx | Bilateral MRND | × | 70/Male | drainage + somatostatin injection |
| 2 | 2003 | Kamasaki N et al. [4] | Tongue | Left RND, Right MRND | 30GY | 78/Female | drainage |
| 3 | 2007 | Tsukahara K et al. [5] | Thyroid gland | Left MRND | × | 72/Female | drainage |
| 4 | 2007 | Tsukahara K et al. [5] | Tongue | Bilateral MRND | × | 76/Male | drainage |
| 5 | 2007 | Bae JS et al. [6] | Thyroid gland | Left SND(level II-IV) | × | 46/Female | drainage |
| 6 | 2007 | Bae JS et al. [6] | Thyroid gland | Left SND | × | 47/Female | drainage |
| 7 | 2009 | Han C et al. [7] | Thyroid gland | Bilateral MRND, Mediastinal | × | 42/Female | drainage |
| 8 | 2010 | Soodin D et al. [8] | Malignant melanoma | Left MRND | × | 65/Female | drainage |
| 9 | 2016 | Singh R et al. [9] | Lower gingiva | Left MRND | × | 61/Female | drainage |
| 10 | 2021 | Kashoob M et al. [10] | Thyroid gland | Bilateral SND (level VI-VII), Left SND (level II-V) | × | 35/Female | drainage + somatostatin injection |
| Case . | Year . | Author . | Primary . | Neck dissection . | Radiation . | Age/Sex . | Treatment . |
|---|---|---|---|---|---|---|---|
| 1 | 2001 | Al Sebein K et al. [3] | Larynx | Bilateral MRND | × | 70/Male | drainage + somatostatin injection |
| 2 | 2003 | Kamasaki N et al. [4] | Tongue | Left RND, Right MRND | 30GY | 78/Female | drainage |
| 3 | 2007 | Tsukahara K et al. [5] | Thyroid gland | Left MRND | × | 72/Female | drainage |
| 4 | 2007 | Tsukahara K et al. [5] | Tongue | Bilateral MRND | × | 76/Male | drainage |
| 5 | 2007 | Bae JS et al. [6] | Thyroid gland | Left SND(level II-IV) | × | 46/Female | drainage |
| 6 | 2007 | Bae JS et al. [6] | Thyroid gland | Left SND | × | 47/Female | drainage |
| 7 | 2009 | Han C et al. [7] | Thyroid gland | Bilateral MRND, Mediastinal | × | 42/Female | drainage |
| 8 | 2010 | Soodin D et al. [8] | Malignant melanoma | Left MRND | × | 65/Female | drainage |
| 9 | 2016 | Singh R et al. [9] | Lower gingiva | Left MRND | × | 61/Female | drainage |
| 10 | 2021 | Kashoob M et al. [10] | Thyroid gland | Bilateral SND (level VI-VII), Left SND (level II-V) | × | 35/Female | drainage + somatostatin injection |
MRND Modified radical neck dissection, RND: Radical neck dissection, SND: Selective neck dissection.
10 cases of chylothorax without chylous fistula associated with head and neck cancer.
| Case . | Year . | Author . | Primary . | Neck dissection . | Radiation . | Age/Sex . | Treatment . |
|---|---|---|---|---|---|---|---|
| 1 | 2001 | Al Sebein K et al. [3] | Larynx | Bilateral MRND | × | 70/Male | drainage + somatostatin injection |
| 2 | 2003 | Kamasaki N et al. [4] | Tongue | Left RND, Right MRND | 30GY | 78/Female | drainage |
| 3 | 2007 | Tsukahara K et al. [5] | Thyroid gland | Left MRND | × | 72/Female | drainage |
| 4 | 2007 | Tsukahara K et al. [5] | Tongue | Bilateral MRND | × | 76/Male | drainage |
| 5 | 2007 | Bae JS et al. [6] | Thyroid gland | Left SND(level II-IV) | × | 46/Female | drainage |
| 6 | 2007 | Bae JS et al. [6] | Thyroid gland | Left SND | × | 47/Female | drainage |
| 7 | 2009 | Han C et al. [7] | Thyroid gland | Bilateral MRND, Mediastinal | × | 42/Female | drainage |
| 8 | 2010 | Soodin D et al. [8] | Malignant melanoma | Left MRND | × | 65/Female | drainage |
| 9 | 2016 | Singh R et al. [9] | Lower gingiva | Left MRND | × | 61/Female | drainage |
| 10 | 2021 | Kashoob M et al. [10] | Thyroid gland | Bilateral SND (level VI-VII), Left SND (level II-V) | × | 35/Female | drainage + somatostatin injection |
| Case . | Year . | Author . | Primary . | Neck dissection . | Radiation . | Age/Sex . | Treatment . |
|---|---|---|---|---|---|---|---|
| 1 | 2001 | Al Sebein K et al. [3] | Larynx | Bilateral MRND | × | 70/Male | drainage + somatostatin injection |
| 2 | 2003 | Kamasaki N et al. [4] | Tongue | Left RND, Right MRND | 30GY | 78/Female | drainage |
| 3 | 2007 | Tsukahara K et al. [5] | Thyroid gland | Left MRND | × | 72/Female | drainage |
| 4 | 2007 | Tsukahara K et al. [5] | Tongue | Bilateral MRND | × | 76/Male | drainage |
| 5 | 2007 | Bae JS et al. [6] | Thyroid gland | Left SND(level II-IV) | × | 46/Female | drainage |
| 6 | 2007 | Bae JS et al. [6] | Thyroid gland | Left SND | × | 47/Female | drainage |
| 7 | 2009 | Han C et al. [7] | Thyroid gland | Bilateral MRND, Mediastinal | × | 42/Female | drainage |
| 8 | 2010 | Soodin D et al. [8] | Malignant melanoma | Left MRND | × | 65/Female | drainage |
| 9 | 2016 | Singh R et al. [9] | Lower gingiva | Left MRND | × | 61/Female | drainage |
| 10 | 2021 | Kashoob M et al. [10] | Thyroid gland | Bilateral SND (level VI-VII), Left SND (level II-V) | × | 35/Female | drainage + somatostatin injection |
MRND Modified radical neck dissection, RND: Radical neck dissection, SND: Selective neck dissection.
Selle et al. reported that over 1500 mL of chyle, unchanged condition after concervative treatment for 14 days, and deterioration of nutrition by chyle exudation were the criteria for surgical intervention [13]. On the other hand, Robinson et al. [14] suggested 500–1000 mL of chyle per day for 2–3 weeks for adults required surgical treatment. Although standardized criteria do not exist, these conditions support our selection of treatment. Moreover, the American College of Radiology recommends lymphangiography and thoracic duct embolization as an effective and minimally invasive method for the treatment of chylothorax [15].
In this case, conservative treatment of low-fat diet improved the patient’s condition after 16 days of thoracentesis. Early diagnosis with adequate treatment is critically important for chylothorax following neck dissection.
Acknowledgements
The authors would like to thank Enago (www.enago) for the English language review.
Author contributions
SK and HY wrote the manuscript. SK, HY and TH were in charge of treatment of this case. HY, KK, AT and YH helped SK with revision of the manuscript. All authors read and approved the final manuscript.
Conflict of interest statement
The authors declare that they have no competing interests.
Funding
None declared.
Data availability
Not applicable.
Consent for publication
Written informed consent for publication of their clinical details and clinical images was obtained from the patient.



