-
PDF
- Split View
-
Views
-
Cite
Cite
William Sergi, Norma Depalma, Tiziana Marchese, Farshad Manoochehri, Stefano D’Ugo, Stefano Garritano, Ivan Botrugno, Ambra Chiappini, Annarita Libia, Carlo Olla Atzeni, Elisa Stasi, Marcello G Spampinato, Robotic-assisted distal pancreatectomy with splenectomy in a paediatric patient for solid pseudopapillary tumour, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad145, https://doi.org/10.1093/jscr/rjad145
Close - Share Icon Share
ABSTRACT
Solid pseudopapillary tumour is a rare low-grade malignant potential carcinoma of the pancreas that typically occurs in females in their third decade. It most commonly occurs in the tail of the pancreas, although any site can be affected. Surgical resection is the standard treatment and offers an excellent prognosis. We report a case of a 17-year-old female with an acute onset abdominal pain and a radiological diagnosis of a cystic lesion in the distal pancreas. A robotic-assisted distal pancreatectomy with splenectomy was performed. Robotic-assisted surgery is an emerging technique for the treatment of pancreatic neoplasms. This approach can be considered for younger patients, thanks to the potential advantages of the robotic Da Vinci Xi System.
INTRODUCTION
Solid pseudopapillary tumour (SPT) of the pancreas is a rare carcinoma estimated to comprise less than 3% of exocrine pancreatic tumours, although, thanks to the increasing in the access to radiological imaging such as computed tomography (CT) or magnetic resonance imaging (MRI), its incidence has been estimated to be up to 6%. Most tumours have areas of necrosis and haemorrhage resulting in both cystic and solid portions [1–2].
These tumours are usually well circumscribed and located in the tail of the pancreas (followed by the head), although an estimated 10–15% of cases are malignant, often involving the liver or peritoneum. The low-grade malignant potential of the tumour leaves it amenable to surgical intervention [2–3].
The first case series of laparoscopic distal pancreatectomies (LDP) for SPT published by Cavallini et al. in 2011 reported the safety and feasibility of the minimally invasive approach as a treatment for SPT, though the technical challenges of laparoscopic pancreatic surgery have resulted in its slow but rising acceptance [4]. Robotic assistance offers several advantages, including increased dexterity and three-dimensional visualization [5]. Herein, we report one of the first use, to our knowledge, of robotic-assisted distal pancreatectomy in a paediatric patient who was diagnosed with a symptomatic distal pancreatic mass.
CASE REPORT
In March 2022, a 17-year-old female with no past medical history was admitted to the Emergency Department with a 5-day history of recurring central quadrant pain and several episodes of emesis. At physical examination, she revealed a non-distended abdomen with minimal tenderness in the central quadrant. Ultrasound showed a well-circumscribed hypoechoic lesion measuring 6.5 cm in diameter near the left hepatic lobe.
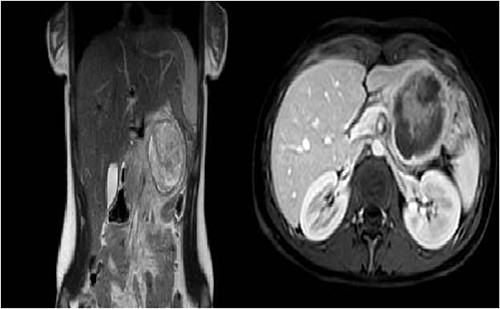
The patient was referred to the Haematology Department and underwent an MRI that showed features consistent with a diagnosis of SPT. After surgical evaluation, the patient was referred to our Department. Preoperative workup included also a thoraco-abdominal CT-scan and normal levels of pancreatic tumour markers (chromogranin A, CA19.9, CA125) (Fig. 1).
After obtaining the informed consent by the patient and her parents, a surgical procedure was planned using the ‘da Vinci Xi’ robotic platform. The patient was positioned in a reverse Trendelenburg position, 15° right tilt with a gel pad placed under the left flank; used the Veress technique, trocar placement was as follows: AirSeal 12-mm trocar (A) in the left iliac fossa, four 8-mm robotic trocars along the umbilical line, 7 mm distant to each other, being the abdominal surface limited due to the paediatric condition (Fig. 2).
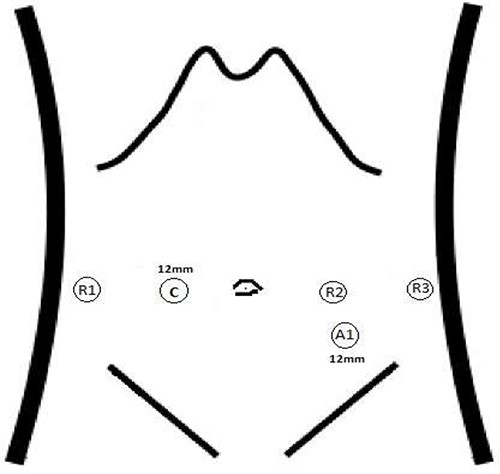
Placement of trocars. The ports for the camera (C), robotic arms (R1–R3) and the assistant port (A) are shown.
Intraoperative blood loss was nil and operating time was 410 min.
Histological examination of the mass confirmed the diagnosis of pT2N0M0 SPT.
Patient was discharged on post-operative day 16 because of ileus and an episode of post-operative vomiting. An urgent CT-scan was performed, revealing a fluid collection in the dissection area that was treated by a percutaneous drainage.
DISCUSSION
Malignant pancreatic tumours are very rare in the paediatric population [6]. Pancreatoblastoma and SPT are the most common epithelial tumours in this cohort of patients, followed by ductal adenocarcinoma, acinar cell carcinoma and pancreatic endocrine neoplasms [7]. The most frequent presenting features of pancreatic tumours are abdominal pain or an upper abdominal mass; jaundice is much less common than in adults [8]. However, over 15% of children with SPT are asymptomatic [1].
The histogenesis of SPT is unclear but they have a higher prevalence in young women, in whom approximately 90% of tumours occur, with a mean age of presentation between 20 and 30 years [1, 2]. Although SPT are typically large (average diameter of 8–10 cm), there is normally no evidence of pancreatic dysfunction or elevated tumour marker levels [9]. The differential diagnosis includes pseudocysts, other cystic neoplasms and secondary tumours of the pancreas, and is often made by performing n abdominal CT scan or MRI. [9]. Surgical resection is the standard of care for SPT. Complete resection of the tumour allows a 5-year survival rate of over 95% [1].
As over 40% of tumours involve the tail of the pancreas, the laparoscopic approach has become the gold standard in distal pancreatectomies as it does not require any reconstruction, thereby reducing the technical difficulties.
A recent meta-analysis by Nigri et al., comparing open distal pancreatectomy with minimally invasive distal pancreatectomy for a variety of benign and malignant lesions, showed that although mortality and re-operative rates did not differ between the two methods, the minimally invasive approach had fewer complications, less blood loss, a faster resumption to oral intake and a shorter post-operative hospital stay [10].
Robotic technology provides further benefits in abdominal surgery, including tremor stabilization, three-dimensional visualization and a wrist-like movement of instruments.
Another advantage of the robotic approach seems to be the reduction in the rate of conversion to laparotomy, as showed by Daoudi et al. [11] reporting a rate of 0 vs. 16% in LDP.
The authors agree with Goh et al. that the bedside assistant should be an expert pancreatic surgeon capable of correctly assisting the first surgeon with suctioning and retraction, as well assisting with rapid conversion to laparotomy if a complication arises [12].
Overall, the authors found the additional operative time incurred with the use of the robotic platform is offset by the numerous advantages listed.
CONCLUSION
The authors report a case of a 17-year-old female with an SPT in the tail of the pancreas that was successfully treated with spleen preserving robotic-assisted distal pancreatectomy. We found that the advantages provided by a robotic approach, including improved surgical dexterity and visualization, allow for its use, as a safe and effective alternative to open pancreatectomy for SPT in paediatric patients.
GUARANTOR
Marcello Spampinato.
PROVENANCE AND PEER REVIEW
Not commissioned, externally peer-reviewed.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No funding was used.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
The work was written in line with the SCARE criteria [1]. Consent to the processing of data for scientific purposes is requested and signed at the time of admission and kept in the medical record; the authors confirm that the patient's parents have signed consent to the publication of the data.
ETHICAL APPROVAL
In our institute, the approval of the ethics committee for the retrospective analysis of a clinical case report is not required.



