-
PDF
- Split View
-
Views
-
Cite
Cite
Neil Jain, Evan Hernandez, Amy Wu, Insufflation via a peritoneal dialysis catheter is a safe way to achieve pneumoperitoneum: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 10, October 2023, rjad599, https://doi.org/10.1093/jscr/rjad599
Close - Share Icon Share
Abstract
A 66-year-old female with a preoperative high index hostile abdomen was incidentally found to have a right T1a 16 mm renal cell carcinoma mass. She safely underwent robot assisted partial nephrectomy after her peritoneal dialysis catheter was alternatively used for insufflation. This adjustment in technique reduced risk related morbidity and possible conversion to open laparotomy.
Introduction
The use of nephron-sparing surgery (NSS) has been recommended as a treatment of choice for T1 renal cell carcinoma as it preserves renal function compared to more radical techniques [1, 2]. Guidelines from the American Urological Association promote nephron sparing approaches as the reference standard for T1 renal cell carcinomas due to the direct link between chronic kidney disease (CKD) and radical nephrectomy (RN) [1, 3]. Techniques that fall under the category of NSS include open partial nephrectomy (OPN), laparoscopic partial nephrectomy (LPN), and robot assisted partial nephrectomy (RAPN) [1, 4]. Previous literature examining these techniques concluded that RAPN is superior to other NSS procedures with improved perioperative, oncological, and renal functional outcomes [4]. Contributing factors include improved dexterity, visualization, quicker recovery times and shorter learning curve [1].
Although RAPN is now emerging as the gold standard for partial nephrectomies, it has a notable complication rate of up to 35% and is subject to the same limitations of laparoscopic techniques [1, 5]. The loss of perception, camera limitations, and difficulty controlling bleeding already make these procedures more technically demanding than other NSS methods [5]. RAPN and laparoscopic surgery may also be further limited due to contraindications in cases where patients have a high preoperative score of 3 or 4 on the Hostile Abdomen Index (HAI) for Laparoscopic Surgery [5]. Patients with higher index scores due to severe comorbidities or prior laparotomies are more likely to possess severe adhesions requiring conversion to further laparotomies [5].
In this report, we present a case where a patient with a preoperative high scoring hostile abdomen safely underwent RAPN for an incidentally found T1a renal mass after insufflation was alternatively achieved using her peritoneal dialysis catheter.
Case presentation
A 66-year-old morbidly obese female with relevant past medical history of type 2 diabetes mellitus, hypertension, and end stage renal disease on peritoneal dialysis (PD) was found to have an incidental enhancing right renal mass concerning for neoplasm on computerized tomography (CT) urogram workup for bacterial peritonitis secondary to streptococcus agalactiae bacteremia (Figs 1 and 2). After appropriate antibiotic treatment and discharge, the patient followed up in clinic where review of the incidental exophytic 16 mm renal mass confirmed suspicions for renal cell carcinoma. The patient still produced urine and was on the transplant list, but wished to proceed with RAPN of the suspicious lesion. A decision was made to use the patient’s PD catheter given her preoperative score of >3 on the Hostile Abdomen Index [5]. In addition to history of bacterial peritonitis, the patient had a notable past surgical history of open cholecystectomy, umbilical hernia repair, and laparoscopic peritoneal dialysis catheter placement in the past 3 months. She was also awaiting a transplant donor, and wished to remain on the list. In the operative theater, her double-cuffed Tenckhoff PD catheter was capped and prepped into the sterile field. Insufflation tubing was connected to the PD catheter and pneumoperitoneum was achieved with normal opening pressure. Laparoscopic trocars were sequentially placed and RAPN was completed without complication. The patient’s post-operative course was unremarkable. Upon physical examination at her 1 month follow-up, her incision sites remained clean, dry, and intact with no complaints of pain. She denied dysuria and gross hematuria. She was cleared to restart peritoneal dialysis at that time. Subsequent pathologic examination of the renal mass confirmed Type 2 Renal Cell Carcinoma with pathologic stage classification T1a, N0 and no signs of regional lymph node metastasis. The patient was instructed to follow-up in 6 months but was ultimately lost to follow-up on our urologic service.
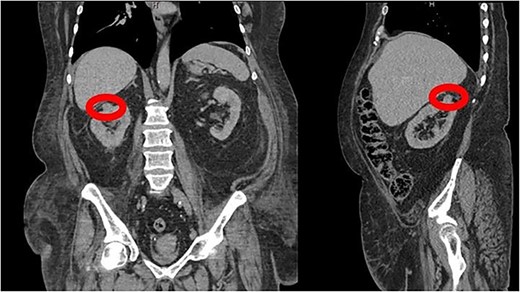
CT Urogram demonstrating a 1.6 cm enhancing right renal mass suspicious for renal cell carcinoma.
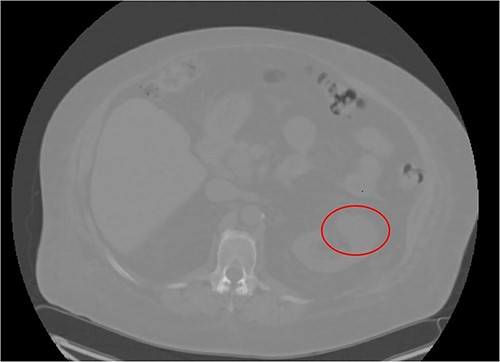
CT Urogram demonstrating right renal mass suspicious for neoplasm.
Discussion
Intraperitoneal access for laparoscopic surgery is traditionally done via the closed Veress Needle method or open Hasson technique. The Veress needle method is a closed technique in which a Veress needle is inserted blindly at an angle ranging from 45° to 90° at the level of the umbilicus to puncture through layers of the abdominal wall [6]. The Hasson method is an open method in which the abdominal wall is incised at the level of the umbilicus [6]. Each of these methods require sufficient access in order to achieve trocar placement and pneumoperitoneum. In Goldfarb et al., the authors reported 43 cases of bleeding complications and 23 inadvertent enterotomies associated with traditional laparoscopic procedures performed from 1998 to 2010 [5]. The authors created the Hostile Abdomen Index (HAI) where it was used to conclude that patients with a preoperative score of 3 and 4 showed a statistically significant increase in these laparoscopic complications [5]. Given our patient’s extensive history of acute peritonitis and multiple abdominal surgeries in the span of a few short months, she was preoperatively determined to be rated >3 on the Hostile Abdomen Index [5]. To reduce risk related morbidity and possible conversion to open laparotomy, we adjusted our technique to utilize the patient’s preplaced PD catheter for insufflation.
To our knowledge, this is the first report making distinct use of a patient’s PD catheter as a method of achieving pneumoperitoneum. However, multiple factors contributed to the successful excision of the patient’s mass. AUA recommendations for our patient with multiple comorbidities are indeterminant [3]. They leave consideration of open versus laparoscopic approaches for partial nephrectomy up to the clinician based on location and size [3]. The patient’s small tumor size with no evidence of metastasis, and her status on the transplant list pushed us toward minimizing risks with RAPN. Prospectively, we suggest additional studies be done to assess whether the risk stratification using PD catheter insufflation is statistically significant among larger power cohorts.
Conflicts of interest statement
The authors have no conflicts of interest to disclose.
Funding
This research received no funds, grants, or other support from agencies in the public, commercial, or not-for-profit sectors.
Declarations
The authors have no conflicts of interest to declare.
Data availability
Access to the data supporting the case report is restricted due to the Health Insurance Portability and Accountability Act. Deidentified data can be provided by the authors upon request.



