-
PDF
- Split View
-
Views
-
Cite
Cite
Annabelle G Ganko, Nicolas Copertino, Late diagnosis of a giant, pedunculated, cutaneous melanoma: a rare case study in an Australian tertiary centre, Journal of Surgical Case Reports, Volume 2023, Issue 10, October 2023, rjad594, https://doi.org/10.1093/jscr/rjad594
Close - Share Icon Share
Abstract
Giant melanomas are uncommon tumours that still occur in Australia despite extensive public health messaging on the importance of early detection of skin cancers. We present the case of a 49-year-old female with a giant melanoma of her left arm measuring 101 × 71 × 22 mm, which had been growing for over 1 year and was metastatic on presentation. In this interesting case, we identify reasons for delayed presentation and highlight the importance of multi-disciplinary care in the management of such large tumours, with reference to other cases in the literature.
Introduction
Rates of cutaneous melanoma in Australia are high, and while the prognosis of advanced melanoma has improved with immunotherapies, 5-year survival remains low [1]. Giant cutaneous melanomas are a rare subset of melanoma defined purely by their size, with a threshold of >10 cm commonly applied [2–4]. Many are metastatic on diagnosis. The treatment of metastatic giant cutaneous melanomas is as for any metastatic melanoma, with the addition of managing the symptoms of such a large tumour. These may include functional limitations as well as bleeding and consequent anaemia [2, 5].
In Australia, there are few barriers to healthcare access and there is significant focus on early detection, through public health campaigns and advances in diagnostic technologies [6]. Despite this, delayed presentations of large metastatic melanomas still occur in Australia.
We present a case of a giant metastatic melanoma at a tertiary hospital in Queensland, Australia and discuss barriers to accessing timely healthcare and the multi-disciplinary management of such advanced cancers.
Written, informed consent was obtained from the patient for publication of this case report and its images.
Case report
A 49-year-old Caucasian female with no significant medical history presented to our General Surgery clinic with a lesion on her left arm. It was in the location of a naevus, which had been present since childhood and had been rapidly enlarging over 1 year. She attributed her delay in seeking treatment to work pressures and thinking the lesion was a wart. Her symptoms were fatigue and discomfort from the tumour. She had no personal or family history of melanomatous skin cancers.
On physical examination, the patient had a large, ulcerated, fungating, pedunculated, brown mass on the posterolateral aspect of her left arm, which was oozing blood (Fig. 1). She had left axillary lymphadenopathy and several subcutaneous nodules in her right arm, chest, and left thigh.

Pre-operative picture of a pedunculated, fungating tumour on the left arm of a 49-year-old female, with surrounding area of discolouration, which was included in the surgical resection.
Haematological investigations revealed microcytic anaemia (haemoglobin 83 g/L, mean corpuscle volume 76 fL) and leukocytosis (white cell count 15.1 × 10^9 cells/L). The remainder of her full blood count was normal.
Staging investigations were completed with a Positron Emission Tomography scan showing pulmonary metastases, disseminated subcutaneous nodular deposits, a likely right inguinal lymph node deposit, and intramuscular metastasis to the left thigh. Computed tomography and magnetic resonance imaging of the head revealed a 16 mm metastatic deposit adjacent to the right ventricle, without mass effect. A bone scan did not show any skeletal metastases.
A palliative resection of the tumour was completed for management of bleeding, anaemia, and discomfort. Under general anaesthetic, a 115 × 80 × 16 mm area of skin was excised from the left posterolateral arm, encompassing both a 101 × 71 × 22 mm mass on a 30 mm-wide stalk and surrounding skin changes concerning for in-transit disease (Fig. 2). A 2:1 meshed, split thickness skin graft was grafted to the wound (Fig. 3). At review 1-week post-operation, the graft had taken and a vacuum assisted closure dressing was applied to assist with wound healing. On subsequent review, the wound had progressed well, and the patient was discharged to her General Practitioner for further wound care.
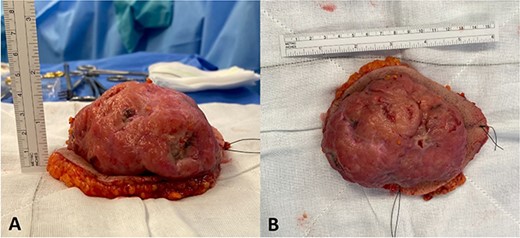
Post-excision pictures of the 101 × 71 × 22 mm tumour. (A) Inferior view (stitch lateral). (B) Anterior view (short stitch superior).

A split thickness, meshed 2:1 skin graft was applied to the left arm wound from a thigh donor site. The graft successfully took to the wound and healed well.
Histopathology confirmed a Clark level 4 nodular melanoma with ulceration and a pathological staging of pT4b pNX cM1d. Breslow thickness was confirmed to be >4 mm, though was difficult to assess due to the markedly exophytic nature of the lesion. There was no reportable BRAF variant detected.
After discussion at the skin cancer multi-disciplinary team meeting, nivolumab/ipilimumab combination therapy was commenced, and the patient was referred to radiation oncology for management of her brain metastasis. In addition to medical treatments, she was referred to psychology, social work, and exercise physiology to assist in managing her metastatic cancer diagnosis.
At time of writing, the patient is still undergoing immunotherapy treatment.
Discussion
There is no formal definition of giant melanomas and thus far most of the literature is comprised of case reports or small case series. The literature includes heterogeneity in size and location. Several reported giant melanomas are nodular, as in this case, which are generally faster growing, have a greater Breslow thickness on diagnosis and are associated with poorer outcomes [7–10]. Many, but not all, have distant metastases on diagnosis [3, 4, 9, 11], as in this case.
Despite their size, management for giant melanomas is principally the same as for regular melanomas [2, 5]. Additional considerations for giant melanomas include approach to skin coverage, functional considerations, and management of symptoms associated with such a large tumour, including the role of palliative resection [3, 12].
In Australia, the majority of diagnosed melanomas are thin melanomas (<1 mm thick), suggesting that many are detected early as a result of the high public awareness of skin cancers in Australia and low barriers to accessing primary care [13]. As in this case, however, delayed presentations do still occur.
Delayed presentation is multifactorial, with age, health literacy, social pressures, and co-morbidities, including psychiatric diseases, all playing a role in progression to a giant melanoma [4, 14]. The patient in this case was fearful of the financial ramifications of time off work if she were to seek medical attention for her tumour. She reported this was exacerbated by recent financial losses due to the COVID-19 pandemic. This highlights the ongoing effects of the pandemic, which has already negatively affected timely skin cancer diagnoses [15].
The patient in this case reported being aware of the dangers of UV radiation and denied excessive sun exposure. She was also aware of the severity of melanomas and some 6 months before seeking medical attention acknowledged to herself that the lesion could be a melanoma. This highlights the necessity for ongoing public heath messaging on melanomas and encouraging people to seek medical attention.
This case also emphasizes the importance of a multi-disciplinary approach to the management of advanced melanomas with social work, psychology, and oncology involved in this patient’s care, in addition to the surgical team. Palliative care will likely play a role in the future too.
This interesting case of a giant melanoma in Australia highlights the ongoing need for education regarding skin cancers in Australia and the social factors which must be navigated with the help of a multi-disciplinary team to optimize health outcomes. Furthermore, this case further exemplifies the persistent and far-reaching ramifications of the COVID-19 pandemic.
Conflict of interest
None declared.
Funding
None declared.



