-
PDF
- Split View
-
Views
-
Cite
Cite
Abigail Jacobs, Tulio Brasileiro Silva Pacheco, Amir Sohail, Anirudha Goparaju, Superior mesenteric artery syndrome secondary to thyrotoxicosis, Journal of Surgical Case Reports, Volume 2022, Issue 9, September 2022, rjac428, https://doi.org/10.1093/jscr/rjac428
Close - Share Icon Share
Abstract
Superior mesenteric artery (SMA) syndrome is defined as a narrowed space and decreased angle between the SMA and aorta leading to partial or complete obstruction of the third portion of the duodenum. SMA syndrome patients may have comorbid conditions associated with extreme weight loss, hypermetabolism or malnutrition. We present the case of a 55-year-old male with SMA syndrome due to acute weight loss secondary to thyrotoxicosis. The patient was nutritionally optimized and euthyroid prior to undergoing a robotic-assisted duodenojejunostomy. In this patient, the thyrotoxicosis was controlled medically, and he remained euthyroid postoperatively. His duodenal obstruction was relieved by the operation and he continued to gain weight appropriately.
INTRODUCTION
Superior mesenteric artery (SMA) syndrome, also known as Wilkie Syndrome, occurs as a consequence of a partial or complete obstruction of the third portion of the duodenum [1]. This obstruction results from rapid weight loss decreasing the thickness of the mesenteric fat pad and subsequently narrowing the angle between the SMA and aorta. The incidence of SMA syndrome is in the range 0.0024–0.3% [2–3]. Known etiologies of SMA syndrome include malignancy, malabsorption, AIDS, burns, bariatric surgery, spinal cord injury, paraplegia, drug abuse, prolonged bed rest and anorexia nervosa [4–7].
The SMA originates from the aorta at the level of the L1 vertebral body, establishing an angle between the SMA and the aorta that ranges from 38 to 65 deg. Radiological findings are crucial in the diagnosis. Criteria include duodenal obstruction with rapid cutoff in the horizontal portion, aortomesenteric artery angle ≤25 deg, aortomesenteric distance ≤8 mm and abnormally high fixation of duodenum by the ligament of Treitz or low SMA origin [8, 9].
We present the case of a 55-year-old male with SMA syndrome due to rapid weight loss secondary to thyrotoxicosis, an etiology that has not yet been described in the literature.
CASE REPORT
A 55-year-old male presented to the emergency room with 2 weeks of intractable vomiting, associated with poor oral intake, diarrhea and 16 kg weight loss. Past medical history, surgical and family history were unremarkable.
The patient was cachectic with a body mass index (BMI) of 19.36 kg/m2 and tachycardic to 102 bpm. His abdominal exam was benign. Computed tomography (CT) scan of the abdomen showed a distended stomach, mild distention of proximal duodenum and a caliber change at the third portion of the duodenum without obstruction. During this evaluation, the patient was tolerating oral intake and was discharged with outpatient follow-up.
Two days later, the patient returned with emesis and poor oral intake. A repeat CT scan of the abdomen and pelvis with IV contrast was notable for increased fluid distention of the stomach and proximal duodenum with an abrupt transition at the level of the narrowed aortomesenteric interval. The aortomesenteric distance measured 5 mm with an SMA angle of 21 deg, confirming SMA syndrome (Figs 1 and 2). He was admitted, started on total parenteral nutrition (TPN). Preoperative endoscopy was performed revealing an area of constriction in the third part of duodenum. The duodenum was dilated without lesions or strictures; however, the endoscope could not traverse this area.
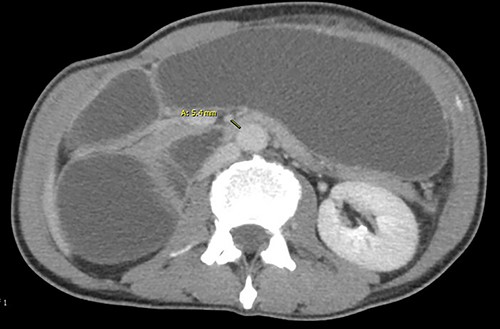

Angle between superior mesenteric and aorta artery measuring 21. deg.
After 9 days of TPN, the patient’s prealbumin increased from 3.9 to 14.2 mg/dl. However, there was inadequate weight gain, tremor and multiple episodes of tachycardia up to 160 bpm. A metabolic workup was consistent with thyrotoxicosis. Thyroid ultrasound demonstrated increased vascularity. Beta blockers and methimazole were initiated. Consideration was given to laparoscopic jejunostomy for outpatient feeding access, but the patient was uninsured. Appropriate home care could not be established and therefore the patient remained inpatient for TPN. After 11 days on antithyroid medication the patient achieved euthyroid status and underwent a robotic-assisted duodenojejunostomy. The patient was discharged on postoperative Day 10 tolerating oral nutrition.
The patient followed as an outpatient over the next 8 months. He reported no postoperative complications and has maintained the euthyroid state. The patient continued to gain weight reaching a BMI of 23.00 kg/m2.
DISCUSSION
SMA syndrome was first described in 1842 by Carl Von Rokitansky, and later Wilkie further categorized its etiology and clinical features [10, 11]. A variety of medical and psychological conditions or surgical interventions may precipitate SMA syndrome as a result of rapid weight loss. SMA syndrome may present as acute or chronic proximal small bowel obstruction. Symptomatology is ambiguous including early satiety and epigastric pain in mild cases. More severe cases can present nausea, bilious emesis and rapid weight loss. Symptomatic relief or improvement in the prone or lateral decubitus position may be indicative of SMA syndrome.
SMA syndrome poses a challenge to providers as the presenting symptoms are often nonspecific. Delay in diagnosis leading to severe morbidity and mortality is not uncommon [1, 3]. The overall prevalence of symptomatic thyrotoxicosis is extremely low, ~0.5% in the USA [12]. In our case the atypical presentation of SMA syndrome in the setting of thyrotoxicosis likely contributed to delayed diagnosis. Therefore, medical providers should be cognizant of the possibility of thyrotoxicosis as an etiology of SMA syndrome.
Conservative treatment of SMA syndrome is based on nutritional optimization aiming to increase the mesenteric fat pad and relieve obstruction [13]. We suggest using National Institute for Health and Care Excellence (NICE) guidelines for assessing nutritional status in adults on TPN, including weekly albumin, and C-reactive protein every 2 to 3 days until stable. Several surgical options exist for SMA syndrome, including Strong’s procedure, feeding jejunostomy, gastrojejunostomy or duodenojejunostomy [14, 15]. Duodenojejunostomy is favored due to the reported success rate between 80 and 100% [14, 15]. Additionally, duodenojejunostomy with division of the fourth part of the duodenum helps to decrease the risk of blind loop syndrome. Our patient underwent a duodenojejunostomy with complete resolution of symptoms and returned to appropriate BMI.
CONFLICT OF INTEREST STATEMENT
None declared.



