-
PDF
- Split View
-
Views
-
Cite
Cite
Shreya Saxena, Deepak Hariharan, Extrapulmonary tuberculosis presentation in the form of a chest wall abscess with no pulmonary involvement in the UK: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 9, September 2022, rjac421, https://doi.org/10.1093/jscr/rjac421
Close - Share Icon Share
Abstract
The presentation of an extrapulmonary manifestation of tuberculous (TB) infection to a tertiary care facility in the UK is a rare event given its low prevalence. This case report focuses on an atypical presentation of an extrapulmonary tuberculosis (EPTB) infection in the form of a chest wall abscess. This was recognized and managed appropriately. This case however elucidates vital learning as migration from around the globe would contribute to an increasing number of TB/EPTB infections. The wide array and indolent nature of their presentation creates diagnostic and treatment challenges. Appreciation for the epidemiology, risk factors, effective and prompt treatment with follow up protocols would help develop pathways for better care. Within the UK, despite it being a low-risk country for TB, there is need for increased awareness, education with established management pathways and governance for TB and EPTB infections.
INTRODUCTION
In 2021, tuberculosis (TB) had the second largest cause of mortality worldwide from an infectious disease after coronavirus disease of 2019, as per the World Health Organization (WHO) [1]. TB is a curable disease and its presentation can be pulmonary and/or extrapulmonary. Extrapulmonary tuberculosis (EPTB) remains a diagnostic challenge and hence awareness amongst clinicians is important to aid recognition, treatment and avoidable mortality.
CASE REPORT
A 31-year-old healthy south-east Asian male presented as a general surgical emergency to a tertiary care facility with a 3-month history of a mass on the right side of his chest. It had progressively increased in size and become painful and erythematous days prior to his presentation. He reported no fevers, shortness of breath, cough, night sweats or weight loss. On examination, it was thought to be a suppurative chest wall abscess (Fig. 1). His inflammatory markers on admission bloods were within normal range. His chest X-ray showed, ‘linear and nodular densities in the right upper zone suggestive of an acute inflammatory process and a new ill-defined density overlying the right lower zone’ (Fig. 2A). Due to concerns of the abscess fungating into the breast or chest wall, he had a computerized tomography (CT) scan of his thorax with contrast. This showed a ‘10 × 4.5-cm mass with internal septations and surrounding fat stranding, arising from the anterior chest wall, with no bony destruction of the fifth anterior rib (Fig. 2B). There were signs of old TB within the lungs with tree-in-bud changes within the right apex suggestive of an acute on chronic infection’.

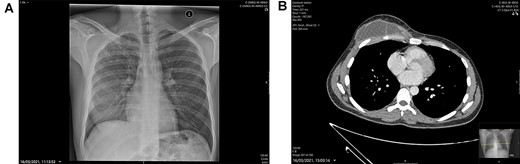
(A) Chest X-ray: linear nodular density right upper lobe. (B) CT Thorax at presentation showing the right-sided anterior chest wall, septating mass highly suspicious of a TB infection.
He had an emergency incision and drainage under general anesthetic. A pus swab was sent for microbiology culture and sensitivity (M, C&S) with acid-fast bacilli testing for TB and biopsy samples sent for histology. He also had a polymerase chain reaction (PCR) test. On discharge, infectious diseases (ID) outpatient follow up was organized to review the culture, PCR and histology result.
The PCR and histology results were both positive for TB. Cultures grew a fully sensitive Mycobacterium tuberculosis bacilli. He was seen in ID clinic and commenced on antitubercular treatment. Initially, he had 2-month intensive therapy of Rifampin, Isoniazid, Ethambutol and Pyrazinamide. The Pyrazinamide was stopped at 6 weeks due to issues with arthralgia. For maintenance therapy he continued for a total 7 months of Rifampin and Isoniazid due to the short course of Pyrazinamide. He had a repeat CT thorax after completing treatment, which showed resolution of the abscess and infection with no evidence of osteomyelitis (Fig. 3).
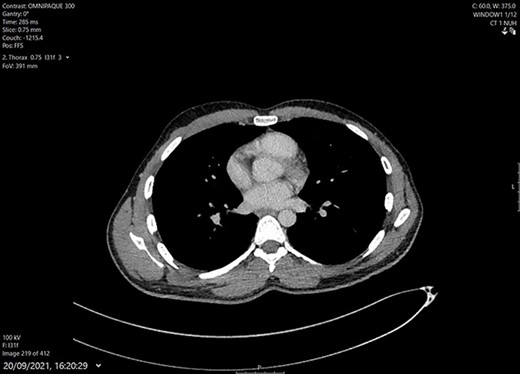
CT Thorax after completing 9 months of medical treatment and surgical debridement of abscess. Shows complete resolution of chest wall mass and intact bony structure underneath.
DISCUSSION
TB can manifest at multiple sites in the body. As per the World Health Organization, EPTB accounts for 16% of TB infections [1]. Of these, 10–35% are musculoskeletal, with 1–5% confined to the chest wall [2, 3]. Hematogenous or lymphatic spread of M. tuberculosis bacilli from the primary infection site, with a cell-mediated immune response results in a granuloma forming. A change in host immunity is thought to reactivate latent TB and present as EPTB [4]. Consequently, being immunocompromised, as well as smoking and excessive alcohol intake are considered risk factors [1, 2]. The classical presentation of chest wall tuberculosis is of an indolent cold abscess, with mildly raised inflammatory markers and few constitutional symptoms [5, 6]. Our patient presented with a predominantly asymptomatic, slow growing abscess. He did not have TB previously. His Bacillus Calmette–Guerine (BCG) vaccination status was unclear. His only risk factor was his south-east Asian ethnicity.
Definitive diagnosis of EPTB is based on positive M. tuberculosis bacilli identification on culture and histology. There is a 10–15% concomitant pulmonary infection with EPTB [7] and therefore, it is recommended all patients have pulmonary involvement determined. Imaging helps assess severity and concomitant infections. In our case, CT was necessary to exclude osteomyelitis and helped exclude any pulmonary disease.
The management of EPTB currently does not differ from that of pulmonary TB. A minimum 6-month course of isoniazid, rifampin, ethambutol and pyrazinamide is still considered the gold standard [7, 8]. There is established guidance on the role of surgery in diagnostic but not curative intent for EPTB. This is particularly evident with musculoskeletal disease presentations. Previous case reports and series found surgical debridement of an abscess may become necessary if there is localized bony involvement, recurrent disease or poor wound healing after completing medical treatment [9–12]. Our patient underwent surgical debridement of his abscess for both diagnostic and therapeutic purposes, which allowed for positive TB identification and timely management of both the abscess and the underlying infection. His post-surgical wound healed well, and he has till date developed no delayed sequelae.
TB is responsible for high mortality rates worldwide [1]. Eight countries (India, China, Indonesia, the Philippines, Pakistan, Nigeria, Bangladesh and South Africa) contribute to the highest TB disease burden, globally [1]. In 2018, six of these countries contributed to 8% of global non-European Economic Area migration into the UK [13]. Studies have found higher incidence of EPTB infections amongst non-UK born citizens [14, 15]. Hence, despite being a low-risk burden country, given the population demographic, an awareness amongst the medical community of TB presentations is essential in the UK.
In conclusion, EPTB is reasonably well known of however, musculoskeletal, and cutaneous involvement is extremely rare and difficult to categorize due to the wide array of presentations associated. This case report aims to help in educating and raising awareness of a rare disease presentation to improve care. There are many documented risk factors for EPTB infections. In this case, the patient’s ethnicity was his only risk factor; however, it was of importance given the epidemiological distribution of EPTB presentations. His presenting complaint could have easily been mistaken for a simple abscess, leading to inappropriate treatment and the possibility of delayed tuberculosis infection sequelae. This case additionally highlights the importance of multi-disciplinary care provision with governance structures. Appropriate and timely referral to the ID team was essential for this patient to receive the appropriate treatment. In having awareness and knowledge on cases such as ours, we help prevent fatality and morbidity from a curable disease.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



