-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammad Alkhatib, Moaaz Alneasan, Widad Aji, Focal myositis in the foot: one unique case in the plantar aspect, Journal of Surgical Case Reports, Volume 2022, Issue 12, December 2022, rjac594, https://doi.org/10.1093/jscr/rjac594
Close - Share Icon Share
Abstract
We present a case of an acquired deformity of the toes of a young patient with no previous pathologic or traumatic history. Later, it emerged that it was ‘Focal Myositis’ at the Flexor Digitorum Brevis muscle of the right foot. The clinical course of the case involved a hard painless mass at the muscle belly that increased in size very slowly over several years, causing flexion contracture of the third toe without an accompanying skin lesion.
INTRODUCTION
Focal Myositis (FM) is a rare inflammatory disease affecting the skeletal muscles, and it is characterized by manifestations that make it difficult to be differentiated from neoplastic malignancies, as it presents as a hard pseudotumor in a single muscle that may be painful or painless, causing a defect in the function or the form of the muscle, and histopathology shows an inflammation with infiltration of inflammatory cells without malignant cells. About 200 cases had been reported as FM; most of them are in the lower extremities. The mechanism of the disease is unknown; it may be pathological, genetic or autoimmune.
CASE REPORT
A 15-year-old boy is brought to the office due to a history of deformity in the third toe of the right foot, observed 6 months ago, that gradually increased in size, causing difficulty for the patient to wear shoes. Medical history shows no trauma to the right foot. The patient’s father noticed that the right foot of his son gradually became larger than the left foot, and he noticed this increase in size 6 years ago. The patient is practicing his daily activities normally without any distinct pain in the right foot. The medical history is unremarkable; there is no illness, allergies or surgery in the patient’s history, but he declares the death of two of his uncles at a young age by an unknown kidney disease.
INVESTIGATIONS
The clinical examination revealed flexion contracture of the third digit of the right foot with dislocation of the proximal interphalangeal (PIP) joint, limited passive and active extension of the second and fourth digits and the presence of little thickness in the skin over the dorsal aspect of the first metatarsophalangeal joint of the foot (Fig. 1). By palpation, there is a non-tender pseudotumor within the plantar aspect of the right foot, without any scare over it (Fig. 2). The X-ray radiographs show inferior dislocation of the PIP joint of the third digit, without any signs of bone lesions or previous fracture (Fig. 3). Ultrasound echomyography shows a significant and heterogeneous increase in the size of the Flexor Digitorum Brevis muscle of the foot. Magnetic resonance imaging (MRI) before gadolinium injuction (Fig. 4) and after gadolinium injuction (Fig. 5) shows a heterogeneous hyperenhancement with irregular margins within the Flexor Digitorum Brevis muscle.
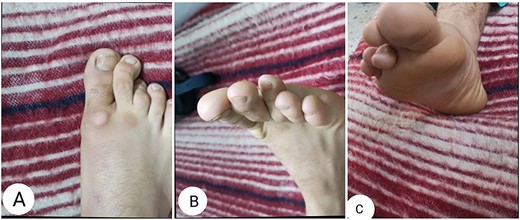
Clinical photographs of the affected foot showing flexion contracture of the third digit.
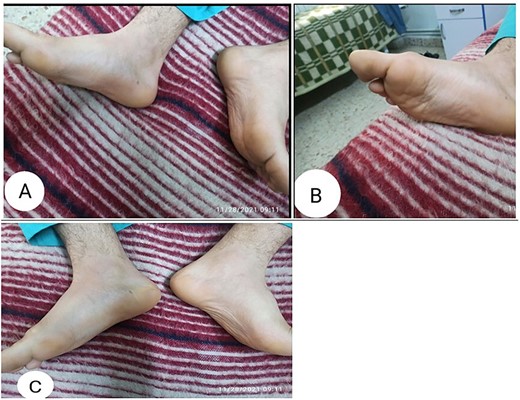
Clinical photographs showing a mass or pseudotumor within the plantar aspect of the right foot.
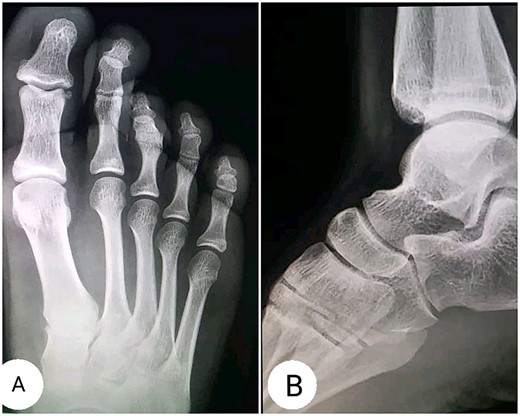
X-Ray radiographs showing (A) inferior dislocation of the PIP joint of the third digit; (B) Lateral radiograph showing no abnormalities.

(A) sagittal T2-weighted, (B) sagittal T1-weighted, (C) axial T1-weighted and (D) Short T1 inversion recovery Magnetic Resonance Imaging (STIR) MRI before gadolinium injection.

(A) sagittal T1-weghited, (B) axial T1-weighted and (C) coronal T1-weighted MRI following gadolinium injection showing hyperenhancement within the muscle tissue.
Laboratory tests are as follows:
ESR: 9 mm/h.
CRP: 3 mg/dl.
LDH: 276 U/L.
Uric acid: 3.3 mg/dl.
Creatinine: 0.7 mg/dl.
Calcium: 10 mg/dl.
The muscle biopsy was performed through a 2-cm incision above the belly of the Flexor Digitorum Brevis muscle, where the muscle fibers appeared visually in pale pink with hypertrophy and the absence of flexibility, but there was an adhesion of the muscle fibers to each other without the presence of damage to those fibers. Histopathology shows degeneration and regeneration of muscle fibers with focal fibrosis associated with interstitial inflammation and focal neurogenic changes. The inflammation consists prominently of eosinophil cells and in some sections there were B cells or CD123+ dendritic plasma cells without the presence of tumor cells (Fig. 6).
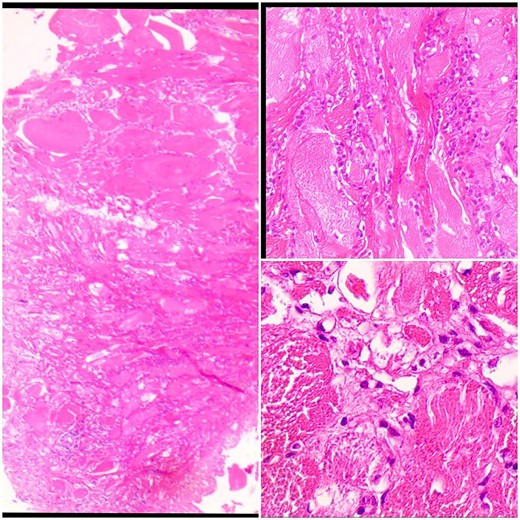
Sections show skeletal muscle fibers infiltrated by inflammatory cells.
DIFFERENTIAL DIAGNOSIS
All clinical manifestations indicated the presence of a muscle-damaging lesion, which made diagnosis challenging. The presence of the mass with the onset of myopathy put the muscular malignancies such as leiomyosarcoma and rhabdomyosarcoma in the differential diagnosis. The findings are non-descriptive for any neoplastic lesion. The most important thing that made the diagnosis confusing in our case was the slow progression, the complete absence of pain and the absence of generalized clinical manifestations. The MRI with contrast, side by side, with the histology is the key point that led to the diagnosis of FM.
TREATMENT
The treatment has been initiated with a single dose of oral corticosteroids ‘prednisolone 20 mg per day’ for a month, and we have noticed a dramatic response to the treatment, as the size and hardness of the pseudotumor have decreased, which prompted us to continue with the same treatment. After that, the dosage of the corticosteroid has been gradually reduced by 2.5 mg every 2 weeks.
OUTCOME AND FOLLOW-UP
After 30 days of corticosteroids administration, the patient was re-examined and there was a significant decrease in the pseudotumor size and hardness and there was a good regression in the contracture of the digit with more flexibility. After 45 days the dosage was reduced to 17.5 mg of prednisone daily. After 60 days the mass size became ~1 × 1 cm with no pain at all. After 120 days, the flexion contracture was resolved by ~90% and the mass was no longer palpable (Fig. 7). At that time, ultrasound echomyography was performed and there were no detectable masses, with the presence of muscle tissue hyperplasia. The patient is under observation until this time.
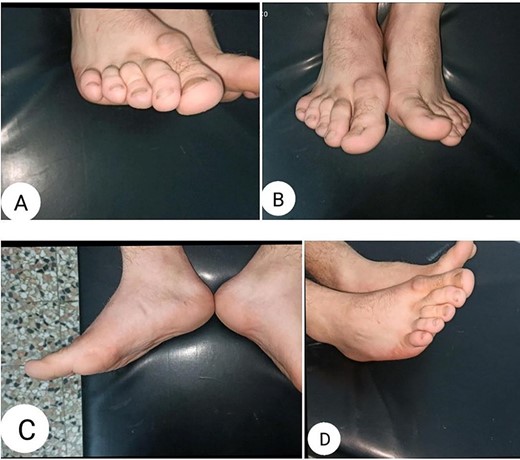
Clinical photographs of the affected foot after 4 months of corticosteroids treatment showing (A, B and D) great resolving of the contracture of the third digit, and (C) almost complete regression of the pseudotumor.
DISCUSSION
FM appeared as a benign inflammatory lesion for the first time in 1977 [1]. Most of the cases were reported in the lower extremity, especially in the thigh and calf, as a painful mass [2]. Several similar cases in the foot were also mentioned, where a case of FM in the small muscles of the foot dorsum was documented and effectively treated with prednisone [3]. FM may turn into multiple myositis after some time in many patients [4]. In the case of our patient, there were no signs of multiple lesions at the time of diagnosis and after up to 6 months of observation. MRI with contrast plays an essential role and provides information that facilitates the diagnosis of FM [5]. This case is one of the rare cases that affect the muscles of the foot and may be the only one that was mentioned in the Flexor Digitorum Brevis muscle. Many muscles have been mentioned in which this injury occurred, such as the muscles of the thigh, pelvic, head and neck [6–8].
In conclusion, FM is a benign, non-neoplastic inflammatory injury that may appear in any muscle of the body and at any age. It is widely misdiagnosed as neoplastic malignancies. It appears as a pseudotumor that may develop quickly or slowly, and maybe painful or painless. MRI with contrast, muscle biopsy and histopathology constitute the cornerstone of the diagnosis. Treatment may include giving steroids or surgery. The injury may decline spontaneously and may develop into multiple myositis.
We have presented a case that may be the first in the medical literature for FM in the Flexor Digitorum Brevis muscle of the foot.
ACKNOWLEDGEMENTS
We are pleased to extend our thanks to Dr. Habib Jarboa for his assistance by providing us with a description of the histopathological sample and a simple explanation that is understandable to the reader at the microscopic level.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
Not applicable.
CONTRIBUTORSHIP
First Author: Mohammad Alkhatib, Diagnosing the case, following up on the patient, conducting the necessary investigations, collecting data, formulating the research and adding the necessary images.
Second Author: Moaaz Alneasan, Data collection, follow-up treatment, translation of the research into English, language revision and collection of samples for histopathology.
Third Author: Widad Aji, Supervising the diagnosis of the case, developing a complete treatment plan, supervising the development of the patient’s condition, collecting data and scientific revision of the research.
INFORMED CONSENT
We had a written consent from the patient.



