-
PDF
- Split View
-
Views
-
Cite
Cite
Christopher J W Shean, Amir Butt, Automatic implantable cardioverter defibrillator (AICD) within the abdomen as a cause of adhesive small bowel obstruction (ASBO): a case report, Journal of Surgical Case Reports, Volume 2021, Issue 9, September 2021, rjab423, https://doi.org/10.1093/jscr/rjab423
Close - Share Icon Share
Abstract
Adhesive small bowel obstruction (ASBO) is commonly caused by intra-abdominal adhesions, usually from prior surgery. Conservative management is the mainstay of treatment, with adhesiolysis required for non-resolving obstruction. An unusual patient presentation of ASBO is presented here, where the cause is proposed as an automatic implantable cardioverter defibrillator (AICD) within the abdomen. Although the patient had several presentations of ASBO successfully treated with conservative management, a non-resolving obstruction required surgical management. At laparotomy, the AICD was found to be in close association with extensive matted adhesions to adjacent small bowel. Adhesiolysis was performed, with the AICD implanted in a subrectus pocket. The patient had an uncomplicated recovery, and at review 6 weeks following the operation was found to have a normal bowel habit with nil further episodes concerning for obstruction. This case highlights the importance of non-classical risk factors being a possible cause of ASBO.
INTRODUCTION
Adhesive small bowel obstruction (ASBO) is one of the most common pathologies admitted to hospital under general surgeons and accounts for up to 75% of all small bowel obstructions in the developed world [1]. Intra-abdominal surgical procedures, especially those involving the lower abdomen or pelvis, are thought to result in the most damage to peritoneal surfaces and places patients at highest risk of subsequent ASBO [2]. Other cause of peritoneal irritation, such as infection, is also known to cause adhesions [3]. Postoperatively inflammation and activation of the coagulation system occurs intending to repair damaged peritoneum, leading to deposition of fibrin and the formation of abnormal fibrous adhesions between tissues that are usually separated [4]. Adhesions are the leading cause of intestinal obstruction in developed countries and result in significant morbidity and mortality. The formation of adhesions varies between patients, but is often dependent on the type and magnitude of surgery, as well as the postoperative course and any complications [3]. The presence of intra-abdominal foreign bodies, ranging from suture material to gallstones, has been shown to contribute to adhesion formation [5], thereby increasing the risk of ASBO. Although the risk factors of intra-abdominal foreign bodies and surgery have been well known for decades, no interventions have been identified that significantly reduce adhesion formation [6]. Conservative management, comprising of making the patient nil by mouth, placing a nasogastric tube, and administering intravenous fluids and electrolytes, is the mainstay of treatment in ASBO, but is contraindicated in patients with peritonitis, signs of ischaemia and strangulation [7]. Although initial conservative management is successful in the majority of cases, ~30% of patients require surgical management to resolve their ASBO [8].
CASE REPORT
An 84-year-old male presented with a 1-day history of abdominal pain in bilateral iliac fossae, associated with nausea, vomiting and last opening his bowels prior to the onset of abdominal pain. Background medical history included rheumatoid arthritis, a prior cardiac arrest, coronary artery bypass graft for ischaemic heart disease, asthma, gout, benign prostatic hypertrophy, atrial fibrillation and gastro-oesophageal reflux. Relevant surgical history included surgical repair of pyloric stenosis as a young child, open appendicectomy in early adulthood, laparoscopic cholecystectomy, placement of an automatic implantable cardioverter defibrillator (AICD) into the abdominal cavity in 2007, and a colonoscopy which identified diverticular disease.
The diagnosis of ASBO was made following a computed tomography (CT) scan of the abdomen and pelvis, which identified a transition point in the pelvis, beam hardening artefact from an AICD within the abdomen, with no underlying mass identified, reported as likely being caused by intra-abdominal adhesions. Conservative management with a nasogastric tube, making the patient nil by mouth and administering intravenous fluids was commenced. The patient opened his bowels and started passing flatus the following day, and then had this diet upgraded. The patient was discharged home after a short admission. A further episode of ASBO a few weeks later was again conservatively managed successfully.
A presentation 6 weeks later was once again diagnosed as ASBO, with multiple segments of dilated small bowel with a transition point identified in the right iliac fossa on CT scan (Figs 1 and 2). On this occasion, operative management was required, with the AICD identified to the left of the umbilicis with extensive matted adhesions to small bowel encountered. Extensive adhesiolysis was undertaken at this area, with the defibrillator removed from the intra-abdominal cavity and repositioned in a subrectus pocket. Following the procedure, the AICD was reactivated and confirmed to be operating as expected. The patient responded well to operative management and began opening his bowels on the third day postoperatively. The patient tolerated a diet and was able to be discharged home. He was reviewed in the clinic 6 weeks after the laparotomy, and at this time it was found he had continued to open his bowels regularly and was undertaking his usual activities with nil issues. The patient had not had any further episodes or symptoms concerning for obstruction.
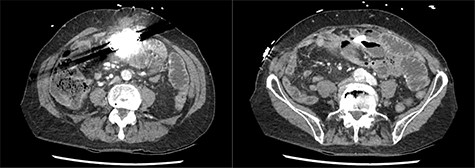
Axial slices of computed tomography scan showing beam hardening artefact from intra-abdominal AICD, adjacent to distended loops of small bowel.
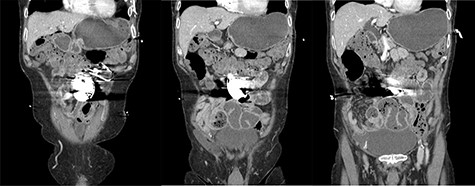
Coronal slices of computed tomography scan shown beam hardening artefact from intra-abdominal AICD, adjacent to distended loops of small bowel.
DISCUSSION
There are currently no published case reports that have investigated a possible link between an AICD within the abdominal cavity and ASBO. Although initial presentations by this patient were successfully managed with conservative measures, during a subsequent presentation surgical management with laparotomy, adhesiolysis and relocation of the AICD foreign body was required. This case presentation illustrates that the mainstay of management principles for ASBO should be maintained even with an unusual causative pathology such as a foreign body causing adhesions, but that in the same manner as all ASBO presentations, surgical management may be required. As populations continue to age, surgical management decisions will have to be made for patients with increasingly complex medical comorbidities, where surgery may be of high risk. Despite no strict contraindications to ongoing conservative management for this patient, with the culprit foreign body remaining in the abdomen, the likelihood of ongoing ASBO may be high, with the elderly patients’ risk at surgical intervention being acceptable due to this ongoing risk of recurrence.
The implantation of an AICD into the abdomen is not common practice; however, this case presentation highlights the importance of considering non-classical risk factors being the cause of an ASBO. Although conservative management is still of use in this situation, surgical management may be required and should still be undertaken in order to reverse the obstruction and prevent further episodes. Current best-practice management protocols indicate the advantage of conservative management in avoiding further adhesion formation following surgery, which then increases risk for further ASBO. In cases such as this with unusual intra-abdominal foreign body being the possible cause of ASBO, this may not be the best clinical decision for the patient. In cases where it is determined the risk of recurrence is higher than the possible disadvantages of surgical management such as additional adhesion formation, surgical management may be the mainstay of treatment rather than ongoing conservative management.
ACKNOWLEDGEMENT
The case report did not receive funding but was performed during the course of employment under the Department of General Surgery, The Canberra Hospital, ACT.
CONSENT
Informed written consent was obtained from the patient that allowed for publishing of the patient history, case details and relevant imaging.
CONFLICT OF INTEREST STATEMENT
There are no conflicts of interest to declare.



