-
PDF
- Split View
-
Views
-
Cite
Cite
Yukihiro Tatekawa, A case of seat belt-induced small bowel rupture and Chance fracture accompanied by elevated serum amylase, Journal of Surgical Case Reports, Volume 2021, Issue 7, July 2021, rjab315, https://doi.org/10.1093/jscr/rjab315
Close - Share Icon Share
Abstract
We report herein our experience with a 10-year-old girl who incurred injuries consistent with seat belt syndrome. The patient was involved in a low-speed motor vehicle accident while restrained in a three-point belt (shoulder and lap belts). She complained of abdominal pain and developed tenderness and abdominal guarding. On admission, enhanced computed tomography (CT) demonstrated a fluid collection in the pelvis and a fractured vertebra in the lumbar spine. The following day, her C-reactive protein and serum amylase levels were elevated and plain CT demonstrated free air in the left side of the abdominal cavity. A ruptured jejunum was detected on laparoscopy. The involved segment of intestine was resected and an end-to-end anastomosis performed. She had an uneventful post-operative course. On post-operative day 14, she was transferred to another facility to undergo therapy for her spinal fracture. After completing conservative therapy, she was discharged 5 weeks after the initial injury.
INTRODUCTION
The ‘seat belt syndrome’ was originally described by Garrett and Braunstein in 1962 [1]. This term refers to the spectrum of injuries associated with lap-belt restraints. The mechanism of hyperflexion and distraction involved in such injuries explains not only thoracolumbar spine dislocations and fractures but also the frequent association of intraabdominal injuries, as the viscera are crushed between the lap belt and the spine [2, 3]. Doersch and Dozier described the ‘seat belt sign’ in 1968, consisting of contusions, petechiae and a band-like pattern of abrasions across the abdomen or chest [4].
The entire class of seat belt-related flexion-distraction injuries to the spine is commonly referred to as Chance fractures. A Chance fracture represents a horizontal splitting of the posterior elements and the body of the vertebra due to seat-belt injury; this specific type of vertebral fracture was described by G. Q. Chance in 1948 [5].
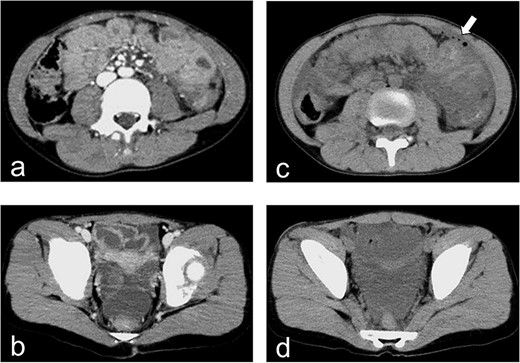
Enhanced and plain CT. (a) Enhanced CT on hospital day 1 demonstrates the absence of free air. (b) Enhanced CT on hospital day 1 demonstrates the presence of a fluid collection in the pelvic cavity. (c) Plain CT demonstrates free air in the left abdominal cavity. (d) Plain CT demonstrates a significant amount of fluid in the pelvic cavity.
Children are more likely than adults to incur combined bone- and soft-tissue injury from a seat belt-related accident [6]. Intra-abdominal injuries resulting from seat-belt trauma include partial- and full-thickness intestinal injuries and mesenteric disruption. In a review of the literature on intra-abdominal trauma secondary to seat-belt injuries, almost every patient had intestinal segment injury. Early diagnosis leads to better outcomes for patients with seat belt injuries, but the diagnosis can be challenging as the typical finding of peritonitis might not be present initially [7].
CASE REPORT
A 10-year-old girl was sitting in the back seat of a right-hand drive car, behind the driver, when another car came from the front and bumped into the patient’s car on the right side. The patient was restrained in a three-point seat belt (shoulder and lap belts). She was transferred to our hospital, where she was alert and communicative on arrival. Her chief complaint was abdominal pain. She was 137-cm tall and weighed 30 kg. On presentation, her heart rate was 87 beats/min, her blood pressure was 123/62 mm Hg, her respiratory rate was 20 breaths per minute, her oxygen saturation was 100% and her temperature was 36.7°C. A seat belt sign was observed, with contusions on the forehead and the right iliac region. Her abdomen was tender and she displayed guarding. Focused assessment with ultrasonography for trauma showed a fluid collection in the pelvic cavity. Enhanced computed tomography (CT) demonstrated no free air but confirmed the presence of a fluid collection in the pelvic cavity (Fig. 1a and b). Radiography and CT showed a fracture of the lumbar spine at L3 (Fig. 2a–c).
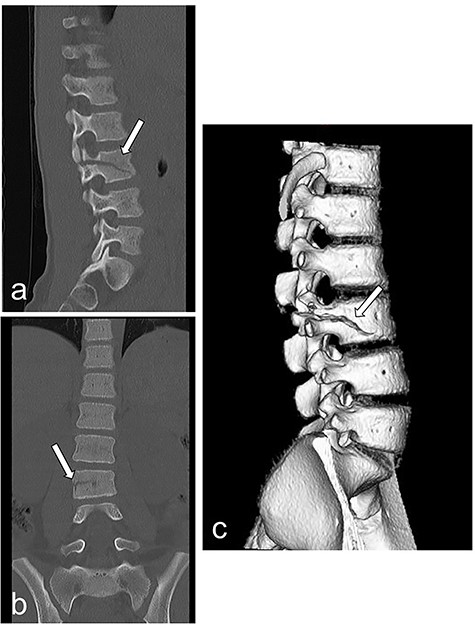
Radiography and CT on hospital day 1. (a, b) Radiography shows fracture of the lumbar spine at L3. (c) CT shows a fracture of the lumbar spine at L3.
The patient was admitted for observation and followed carefully for suspected intestinal injury. The following day, she was tachycardic and febrile, and her abdomen was tender with guarding. Her C-reactive protein level increased from 0.08 mg/dL on the day of admission to 6.92 mg/dL on hospital day 2 (Table 1), while her serum amylase level increased from 132 to 319 IU/L (Table 1). Plain CT demonstrated free air in the left abdominal cavity and a significant fluid collection in the pelvic cavity (Fig. 1c and d). We diagnosed an intestinal injury and performed exploratory laparoscopic surgery.
| . | Day 1 . | Day 2 . | Day 3 . |
|---|---|---|---|
| . | On admission . | On admission . | On admission . |
| . | . | (Operative Day) . | (Postoperative Day 1) . |
| WBC (×103) | 16.2 | 11.2 | 7.6 |
| (/mm3) | |||
| RBC (×104) | 458 | 451 | 396 |
| (/mm3) | |||
| Hb | 13.8 | 13.4 | 11.6 |
| (g/dL) | |||
| Ht | 39.3 | 38.6 | 34.3 |
| (%) | |||
| Plts (×104) | 35.1 | 25.7 | 22.2 |
| (/mm3) | |||
| T-Bil | 0.5 | 1.0 | 0.8 |
| (mg/dL) | |||
| AST | 33 | 57 | 45 |
| (IU/L) | |||
| ALT | 16 | 19 | 19 |
| (IU/L) | |||
| LDH | 305 | 426 | 234 |
| (IU/L) | |||
| AMY | 132 | 319 | 67 |
| (IU/L) | |||
| CRP | 0.08 | 6.92 | 20.93 |
| (mg/dL) | |||
| Amylase in ascites fluid | 8757 | ||
| (IU/L) |
| . | Day 1 . | Day 2 . | Day 3 . |
|---|---|---|---|
| . | On admission . | On admission . | On admission . |
| . | . | (Operative Day) . | (Postoperative Day 1) . |
| WBC (×103) | 16.2 | 11.2 | 7.6 |
| (/mm3) | |||
| RBC (×104) | 458 | 451 | 396 |
| (/mm3) | |||
| Hb | 13.8 | 13.4 | 11.6 |
| (g/dL) | |||
| Ht | 39.3 | 38.6 | 34.3 |
| (%) | |||
| Plts (×104) | 35.1 | 25.7 | 22.2 |
| (/mm3) | |||
| T-Bil | 0.5 | 1.0 | 0.8 |
| (mg/dL) | |||
| AST | 33 | 57 | 45 |
| (IU/L) | |||
| ALT | 16 | 19 | 19 |
| (IU/L) | |||
| LDH | 305 | 426 | 234 |
| (IU/L) | |||
| AMY | 132 | 319 | 67 |
| (IU/L) | |||
| CRP | 0.08 | 6.92 | 20.93 |
| (mg/dL) | |||
| Amylase in ascites fluid | 8757 | ||
| (IU/L) |
| . | Day 1 . | Day 2 . | Day 3 . |
|---|---|---|---|
| . | On admission . | On admission . | On admission . |
| . | . | (Operative Day) . | (Postoperative Day 1) . |
| WBC (×103) | 16.2 | 11.2 | 7.6 |
| (/mm3) | |||
| RBC (×104) | 458 | 451 | 396 |
| (/mm3) | |||
| Hb | 13.8 | 13.4 | 11.6 |
| (g/dL) | |||
| Ht | 39.3 | 38.6 | 34.3 |
| (%) | |||
| Plts (×104) | 35.1 | 25.7 | 22.2 |
| (/mm3) | |||
| T-Bil | 0.5 | 1.0 | 0.8 |
| (mg/dL) | |||
| AST | 33 | 57 | 45 |
| (IU/L) | |||
| ALT | 16 | 19 | 19 |
| (IU/L) | |||
| LDH | 305 | 426 | 234 |
| (IU/L) | |||
| AMY | 132 | 319 | 67 |
| (IU/L) | |||
| CRP | 0.08 | 6.92 | 20.93 |
| (mg/dL) | |||
| Amylase in ascites fluid | 8757 | ||
| (IU/L) |
| . | Day 1 . | Day 2 . | Day 3 . |
|---|---|---|---|
| . | On admission . | On admission . | On admission . |
| . | . | (Operative Day) . | (Postoperative Day 1) . |
| WBC (×103) | 16.2 | 11.2 | 7.6 |
| (/mm3) | |||
| RBC (×104) | 458 | 451 | 396 |
| (/mm3) | |||
| Hb | 13.8 | 13.4 | 11.6 |
| (g/dL) | |||
| Ht | 39.3 | 38.6 | 34.3 |
| (%) | |||
| Plts (×104) | 35.1 | 25.7 | 22.2 |
| (/mm3) | |||
| T-Bil | 0.5 | 1.0 | 0.8 |
| (mg/dL) | |||
| AST | 33 | 57 | 45 |
| (IU/L) | |||
| ALT | 16 | 19 | 19 |
| (IU/L) | |||
| LDH | 305 | 426 | 234 |
| (IU/L) | |||
| AMY | 132 | 319 | 67 |
| (IU/L) | |||
| CRP | 0.08 | 6.92 | 20.93 |
| (mg/dL) | |||
| Amylase in ascites fluid | 8757 | ||
| (IU/L) |
Laparoscopic inspection revealed purulent ascites with intestinal adhesions (Fig. 3a). The amylase level in the ascitic fluid was 8757 IU/L (Table 1). The intestine was pulled out through the umbilical wound, and a segment of the jejunum was confirmed to be ruptured (Fig. 3b and c). The involved 10-cm segment of jejunum was excised (Fig. 3d), and an end-to-end anastomosis was performed.
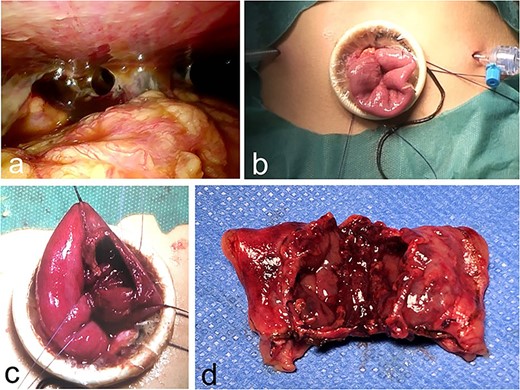
Intra-operative findings. (a–c) Exploratory laparoscopy reveals purulent ascites with intestinal adhesions and a ruptured jejunum. (d) A 10-cm segment of jejunum is excised.
The patient underwent an uneventful postoperative course and was transferred to another facility on postoperative day 14 to undergo physical therapy for her spinal fracture. After completing conservative therapy, she was discharged 5 weeks after the original seat-belt injury.
DISCUSSION
Spinal and intra-abdominal injuries can occur when a school-aged child is involved in an accident while restrained by a seat belt. The impact of a relatively high-riding restraint compresses the fixed duodenum against the lumbar spine, leading to a high rate of injury [6]. Reviews of seat belt-induced injuries to the jejunum and ileum classify these injuries into three groups. In Group I, there is complete transection of the proximal jejunum caused by deceleration forces. Commonly associated injuries include splenic rupture and perforation of the transverse colon and splenic flexure. In Group II, crush injuries result in an infarcted ileum. Associated injuries include tears to the cecum, aorta and inferior vena cava. In Group III, there are ‘blowout’ perforations of the jejunum and ileum [8]. Our patient had a Group III injury involving the jejunum, without splenic trauma or colon injury. We think that her shoulder belt running from the upper right to the lower left, or her lap belt, might have compressed the fixed portion of the duodenum (proximal to the ligament of Treitz) against the lumbar spine.
Our patient had an increased serum amylase level on the second day after incurring seat-belt trauma. In general, an increase in amylase levels is seen in the setting of acute pancreatitis or pancreatic injury. However, it is well known that an abnormal rise in serum amylase levels may occur with a gastrointestinal perforation [9, 10]. The rise in serum amylase in patients with perforated ulcers is probably a result of increased liberation of pancreatic secretions into the peritoneal cavity, with resultant uptake by the lymphatic system. It is suggested that elevated amylase levels can result from large amounts of intraabdominal fluid and large perforations of the bowel [9]. Indeed, we observed a large fluid collection in our patient’s pelvic cavity that increased in size on the second day after a seat-belt trauma. In our patient, neither plain nor enhanced CT revealed a pancreatic injury; therefore, the elevated serum amylase level was deemed to be the result of non-pancreatic disease. Perforation of the small bowel or rupture caused by a seat-belt injury should be considered in the differential diagnosis of patients with abdominal pain accompanying an increasing serum amylase level.
AUTHOR DISCLOSURE STATEMENT
The author has no competing financial interests or funding in connection with this manuscript.
CONFLICT OF INTEREST STATEMENT
The author has no conflicts of interest to declare. The author alone is responsible for the content of this manuscript.



