-
PDF
- Split View
-
Views
-
Cite
Cite
Francisco Navarro, Lissette Leiva, Enrique Norero, Acute abdomen due to pancreatic pseudocyst with splenic extension and rupture, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjab071, https://doi.org/10.1093/jscr/rjab071
Close - Share Icon Share
Abstract
Pancreatic pseudocyst is a common complication of acute and chronic pancreatitis. However, spleen involvement in pancreatitis is rare. We present a patient with a pancreatic tail pseudocyst with splenic extension and rupture. Due to initial stability, conservative management was decided. However, he developed tachycardia with severe abdominal pain associated with signs of peritoneal irritation, requiring an emergency laparotomy. A large pancreatic tail pseudocyst was identified in addition to a ruptured spleen. Splenectomy and double layer hand-sewn gastrocystic anastomosis were performed. The patient had a satisfactory recovery and was discharged on the 11th postoperative day. Conservative management is an option in stable patients but with a high rate of failure. Surgery remains the standard choice in these cases.
INTRODUCTION
Pancreatic pseudocyst is a complication of acute and chronic pancreatitis. It has an incidence of 14% secondary to acute pancreatitis and 41% for chronic pancreatitis [1]. Usually is located in the peripancreatic area but can expand through tissues into areas far away from the pancreas like the liver, spleen, mediastinum and pelvis [2].
Due to anatomical and vascular proximity, pancreatitis may course with splenic complications, including splenic vein thrombosis, subcapsular hematoma, infarction, rupture and intrasplenic pseudocyst [3]. However, the spleen is rarely involved in complications due to chronic pancreatitis [2].
This article aims to describe an unusual case of pancreatic pseudocyst with splenic extension and rupture.
CASE REPORT
A 26-year-old man with a history of 3 years of excessive alcohol intake was admitted to the emergency department for 48 h of abdominal pain, mainly in the left hypochondrium associated with fever and vomiting. He had a history of 1 year of intermittent abdominal pain that intensified over the last month, which led him to stop alcohol consumption. He was hemodynamically stable upon admission. Laboratory test showed C-reactive protein 176 mg/dl, white cell count 16.7 × 109/L, platelet count 617 × 109/L and serum amylase level 109 U/L. The computed tomography (CT) showed a cystic lesion in the pancreatic tail of 5.7 × 9 cm in size and significant splenomegaly with hypodense areas consistent with a pseudocyst with splenic extension and rupture (Fig. 1).
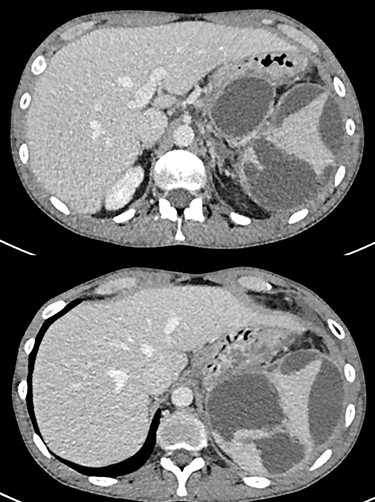
Pancreatic pseudocyst associated with intrasplenic extension and rupture with subcapsular hematoma.
Due to patient stability, conservative management was decided. This included analgesics, antibiotics and nutritional optimization. During the first 48 h, the patient was stable, with little pain and without fever. On the fourth day of hospitalization, he developed tachycardia and severe pain. The abdominal examination showed signs of peritoneal irritation and laboratory tests with a white cell count of 41 × 109/L. Ultrasound assessment showed diffuse abdominal free fluid. An emergency laparotomy was performed, finding 1.5 L of dark serohematic and purulent fluid in the peritoneal cavity. The amylase level of this fluid was 3000 U/L. A large pancreatic tail pseudocyst was identified in addition to abundant clots in the left subphrenic space because of a ruptured spleen (Fig. 2). Due to extensive peripancreatic inflammation, dissection was difficult. Splenectomy was performed, extracting the shattered splenic parenchyma (Fig. 3). The amylase level of pancreatic cystic fluid was 13 000 U/L, confirming the diagnosis of a pseudocyst. We performed a double layer hand-sewn gastrocystic anastomosis with silk 2.0. One drain was located close to the anastomosis and two in the splenic bed. The patient had a satisfactory recovery, with drains fluid amylase level in the normal range, and was discharged on the 11th postoperative day.
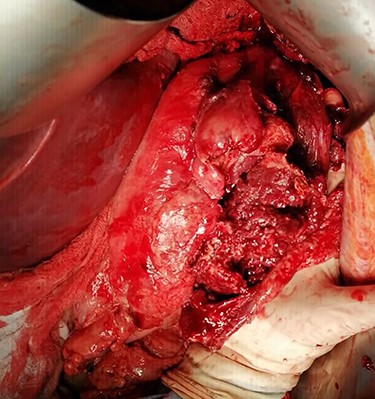
Intraoperative image of the ruptured spleen associated with abundant clots.

DISCUSSION
The anatomic proximity between the pancreatic tail and splenic hilum leads to potential complications in splenic parenchyma due to pancreatitis. Some mechanisms to explain it have been formulated, including erosion of splenic parenchyma resulting from pancreatic enzymes leakage, disruption of splenic hilar vessels and expansion of pancreatic pseudocyst to the spleen [4]. The most common cause of chronic pancreatitis and pseudocyst is alcohol [5].
The splenic involvement in pancreatitis is uncommon. The incidence of splenic complications in chronic pancreatitis has been described in 2.2% in previously reported series [3]. Splenic infarcts and subcapsular hemorrhage are complications more common in acute pancreatitis, and necrotizing pancreatitis and pseudocyst of the pancreatic tail are most frequently associated with splenic complications [2]. Intrasplenic pancreatic pseudocyst is often originated by direct expansion of distal pancreatic pseudocyst and is developed in almost 6% of patients with chronic pancreatitis and distal pancreatic pseudocyst, according to the previous series [5].
Clinical features include nonspecific symptoms including abdominal pain, fever, nausea, vomiting, weight loss and palpable mass [5, 6]. Laboratory tests in patients with pancreatic pseudocysts are often not useful for discriminating if the spleen is involved or not. Diagnosis of pancreatic pseudocyst involving the spleen can be suspected by ultrasound and CT, although the preferred method is the latter [7]. The most common findings are nonspecific hypodense areas that need to be correlated with clinical and history details to confirm the diagnosis.
The management options include conservative treatment, percutaneous or endoscopic drainage and surgery. In patients hemodynamically stable with improving symptoms, the nonoperative approach can be a suitable alternative, as in our case initially. Nevertheless, the spontaneous resolution of intrasplenic pseudocyst is very unusual [8].
External drainage is also described as a treatment in selected circumstances [5]. It has been reported mainly in cases where there is no communication between the pancreatic duct and pseudocyst, due to a high failure rate (33%) [5].
Endoscopic transpapillary drainage is feasible as well, especially in patients when pancreatic duct and pseudocyst are communicated [9]. In previously reported series, the resolution rate was higher than 70%, and success predicting factors were pseudocyst with no infection, with partial ductal disruption, no solid necrotic debris and that the disruption can be bridged by an endoprosthesis [10]. Globally, about 40% of patients managed nonoperatively initially will require surgery [5].
Regarding the surgical management, distal pancreatectomy plus splenectomy can be considered an option for pancreatic cyst with splenic involvement [6]. The addition of distal pancreatectomy to splenectomy allows reducing the rate of pancreatic fistula [3]. The main reported complications are infection, postoperative bleeding and drain tract fistula [5]. However, in the setting of an acute abdomen in a patient with an emergency laparotomy and severe inflammatory adhesion in the peripancreatic region, we believe that splenectomy combined with a cystogastrostomy is a better option that requires less extensive dissection and presents a similar satisfactory outcome.
CONCLUSIONS
Splenic pseudocysts are a rare complication of pancreatitis. The clinical findings are nonspecific, and the diagnosis is confirmed with the CT. Conservative approach is an option in several stable patients but with a high rate of failure. The external or endoscopic drainage can be feasible under certain conditions, and surgery remains the standard choice for unstable patients or with failure to previous methods.



