-
PDF
- Split View
-
Views
-
Cite
Cite
Agustin E Pinsak, Diana A Pantoja Pachajoa, René M Palacios Huatuco, Germán R Viscido, Facundo I Mandojana, Alejandro M Doniquian, Ileocecal intussusception as the initial presentation of endometriosis: case report, Journal of Surgical Case Reports, Volume 2021, Issue 12, December 2021, rjab556, https://doi.org/10.1093/jscr/rjab556
Close - Share Icon Share
Abstract
Cecal endometriosis is a rare entity that can present as nonspecific acute abdominal pain and can be complicated by ileocolic intussusception, which is extremely infrequent. We present the case of a 33-year-old woman with no relevant pathological antecedents who consulted for abdominal pain for 5 days, associated with rebound tenderness and abdominal guarding on the right lower quadrant and a palpable mass during the physical examination. Computed tomography was realized and emergency surgery performed due to suspected ileocolic intussusception. The laparoscopic examination identified an ileocolic intussusception associated with a tumor. Conversion to open surgery was needed, and an oncological right hemicolectomy with ileotransverse anastomosis was carried out. Histopathological study reported ileocolic intussusception and a focus of cecal endometriosis. Currently, the patient does not have recurrences. Ileocolic intussusception secondary to deep endometriosis requires great diagnostic presumption in women of childbearing age with acute abdomen diagnosis.
INTRODUCTION
Ileocolic intussusception due to cecal endometriosis is an extremely rare entity [1]. The intestinal localization of endometriosis is generally in the rectum or sigmoid colon, although it can have an unusual presentation affecting the appendix, ileum and right colon [2, 3]. We present a case of ileocolic intussusception as the initial presentation of endometriosis in a woman of childbearing age.
CASE REPORT
A 33-year-old woman was admitted to the emergency room (ER) with abdominal pain lasting 5 days. The patient did not present comorbidities, previous abdominal surgeries or pregnancies. She reported that the abdominal pain started in the epigastrium and later migrated, localized and intensified in the right lower quadrant (RLQ). It was associated with constipation and poor flatus elimination. The symptoms were not related to menses.
On admission, the patient presented a pulse of 65 beats/min, blood pressure of 140/90 mm Hg, and temperature of 36.5°C. On physical examination, rebound tenderness and abdominal guarding were recognized in the RLQ, and a palpable mass was identified.
Blood tests showed leukocytosis 12 × 109/L with 75% segmented neutrophils, C-reactive protein 8 mg/dL and hemoglobin of 14.2 g/dl. Human chorionic gonadotropin hormone beta-subunit 2.0 mUl/ml. Levels of serum CA 19–9 2.0 U/ml, and carcinoembryonic antigen 0.5 mg/ml. Metabolic panel and liver function tests were within normal limits.
Abdominal ultrasound showed in the ascending colon, a heterogeneous mass composed of a conglomerate of intestinal loops measuring 10 × 8 × 5 cm.
Computed tomography (CT) of the abdomen and pelvis with oral and intravenous contrast was performed (Fig. 1), and emergency surgery was decided due to the suspected ileocolic intussusception with a probable tumor origin (Fig. 2). The preoperative diagnoses were malignant cecum tumor (adenocarcinoma, sarcoma) or benign tumor (lipoma, villous tumor).

Abdominal CT with oral and IV contrast, axial view; tumoral mass and intussusception (arrow).

Abdominal CT with oral and IV contrast, coronal view; tumoral mass and intussusception (arrow).
The initial approach was laparoscopic, recognizing a tumor in the cecum associated with ileocolic intussusception. The abdominal cavity was explored without detecting other foci of probable neoplastic origin. However, due to technical difficulties, the decision was made to convert to conventional surgery. Due to the appearance of the lesion and the suspicion of a malignant tumor, an oncological right hemicolectomy was performed with ileotransverse manual anastomosis (Fig. 3). The operative time was 3 hours, with an estimated blood loss of 100 cm3. It did not require red blood cell units.

Surgical specimen; red circle indicating tumoral mass and vestiges of the intussusceptive process.
The immediate postoperative follow-up was carried out in the intensive care unit. Later the patient went to the inpatient room, where she remained for eight days.
The microscopic study reported ileocolic intussusception and cecal endometriosis (Figs 4 and 5).
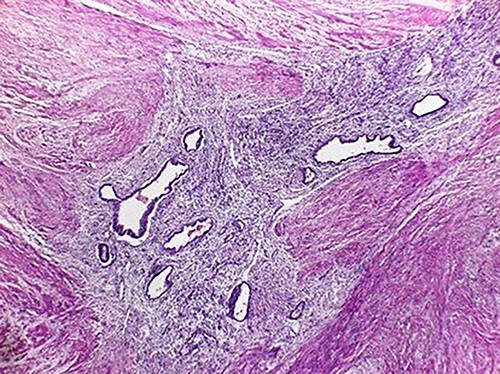
Low magnification image (4x); endometrial glands and stroma in the middle of the external muscular layer of the colon.
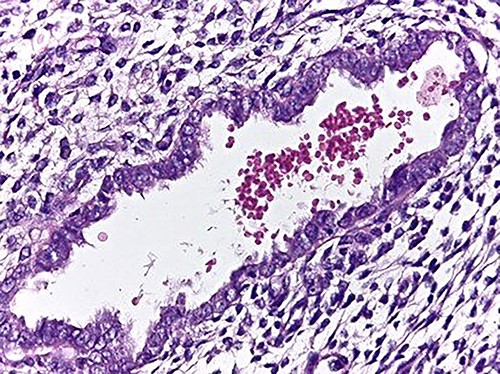
High magnification image (40x); endometrial gland and stroma without atypia. Erythrocytes within the lumen of the gland.
Periodic clinical controls were performed. Five years after surgery, the patient continues under follow-up without presenting new foci of endometriosis.
DISCUSSION
Intestinal intussusception is caused by the extension of an intestinal segment (intussusceptum) into the lumen of the contiguous intestinal tract (intussuscipiens) as a result of impaired motility [4]. According to its location, it is classified as enteric, colonic, ileocecal and ileocolic [5]. An uncommon cause of intussusception is intestinal endometriosis, affecting 3.8–37% of women with endometriosis [2]. The predominant location of endometriosis is at the rectum or sigmoid colon (72%), with a lower percentage in the small intestine (7%), cecum (3.6%) and appendix (3%) [3].
In our case, the patient presented deep cecal endometriosis.
The main symptoms are nonspecific with abdominal pain, dysmenorrhea and dyspareunia. In cases of bowel involvement, the major symptoms could be cramping, dyschezia, cyclic rectal bleeding, diarrhea and obstipation. Bowel endometriosis may be presented as acute abdomen and occlusion due to intussusception or compression [7]. During the anamnesis, our patient did not report gastrointestinal symptoms related to menses.
Multislice CT enteroclysis is recommended, which identifies 94.8% of intestinal endometriotic nodules [8] as well as magnetic resonance imaging, which has a sensitivity of 77–93% [9]. In our case, CT allowed us to identify the ileocolic intussusception. However, the diagnosis of endometriosis was obtained in the delayed histopathology study, so it was not considered in the differential diagnoses.
The treatment and follow-up of patients with deep endometriosis, especially those with involvement of the urinary and/or intestinal tract, and/or multi-operated history, is recommended to be carried out in specialized third-level centers.
Surgical treatment for deep endometriosis is indicated in cases of pain, bleeding and intestinal obstruction. Standard right hemicolectomy with ileotransverse anastomosis has been reported as the most appropriate treatment, either through a laparoscopic or conventional approach. In our case, the initial approach was laparoscopic, with subsequent conversion to open surgery due to technical difficulties. An oncological right hemicolectomy was performed due to the suspicion of a malignant tumor.
The high recurrence rate of endometriosis and its symptoms must be kept in mind, and concomitant medical treatment should be considered in the long-term follow-up in the context of a chronic disease. The follow-up should be clinical (anamnesis and physical examination) and by means of complementary tests depending on the severity and the affected organ. CA-125 is the main serum marker used in the diagnosis and treatment of late-stage endometriosis and is used to monitor the progress of endometriosis [10]. Currently, our patient continues under clinical and biochemical follow-up with no findings of recurrence.
In conclusion, Ileocolic intussusception due to cecal endometriosis is an extremely rare condition that requires a high degree of diagnostic suspicion in women of childbearing age with acute abdomen diagnosis.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- abdominal pain
- acute abdomen
- computed tomography
- physical examination
- endometriosis
- anastomosis, surgical
- laparoscopy
- surgical procedures, operative
- abdomen
- cecum
- diagnosis
- neoplasms
- colectomy, right
- rebound tenderness
- ileocolic intussusception
- ileocecal intussusception
- histopathology tests
- emergency surgical procedure



