-
PDF
- Split View
-
Views
-
Cite
Cite
Nguyen Tran, Valerie-Sue Emuakhagbon, Bradford T Baker, Sergio Huerta, Re-assessing the role of the fecalith in acute appendicitis in adults: case report, case series and literature review, Journal of Surgical Case Reports, Volume 2021, Issue 1, January 2021, rjaa543, https://doi.org/10.1093/jscr/rjaa543
Close - Share Icon Share
Abstract
Appendicitis in adults is thought to occur because of luminal obstruction from a fecalith. We present a unique case of a patient who had her entire appendiceal lumen occupied by a fecalith (5.0 cm long) but had no appendicitis. We reviewed the records of 257 veterans who underwent surgical intervention at our institution for the management of acute appendicitis. Fecaliths occurred in 15.6% of patients. At laparotomy, 20.6% had a perforated appendix; pathology showed fecaliths in 20.8% of specimens. A review of the literature inclusive of 25 series showed fecaliths in 33.3% of patients with a normal appendix, 23.5% of patients with acute appendicitis and 24.9% with perforated appendicitis. These data show that appendicitis is not a common cause of fecalith obstruction in adults.
INTRODUCTION
Conventional teaching in the pathophysiology of acute appendicitis in adults dictates luminal obstruction from a fecalith (or less likely from foreign bodies, parasites, and tumors), which leads to stasis, bacterial overgrowth, inflammation, ischemia and perforation [1]. However, this classic concept, first proposed by Fitz and Mattestock [2], has been questioned by investigators demonstrating a wide range of fecaliths in patients with appendicitis (1.4–67.0%) [3].
Further, intraoperative management of appendiceal pressure in patient with appendicitis revealed that the inflammatory process might be the culprit of luminal obstruction rather than obstruction leading to inflammation [3]. Thus, there is a competing theory that obstruction is the result of inflammation and not the other way around [4].
The classical teaching of a fecalith leading to appendicitis has been challenged by several investigators [4–6], but it has not been systematically analyzed. Current strategies in the management of acute appendicitis include non-operative management (NOM), but fecaliths have been shown to be a predictor of failure to NOM [7]. Thus, a re-assessment of its role in acute appendicitis is timely.
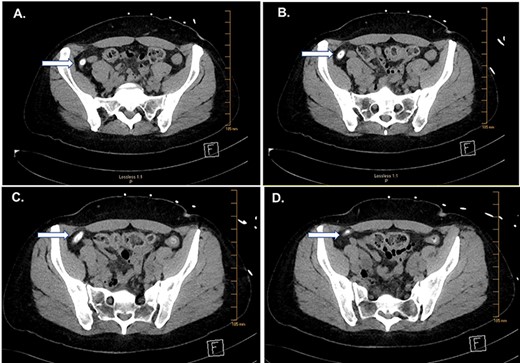
CT of the abdomen and pelvis. Serial images (A–D) from cephalad to caudal show a large fecalith (arrows).
In the present report, we present a unique patient with a very large fecalith occupying the entirety of the appendiceal lumen; we reviewed all appendectomies in our institution for the past 12 years to assess the role of fecaliths in appendicitis. We then reviewed the literature.
CASE REPORT
A 50-year-old veteran woman presented to the emergency department (ED) with a 1-day history of abdominal pain, nausea and multiple episodes of vomiting. Her pain was intermittent, severe and poorly localized to the right lower quadrant. She had had similar episodes necessitating ED visits in the past several months, and pain medication had been prescribed, which improved her symptoms. Her past medical history is significant for inflammatory bowel disease, gastroesophageal reflux disease, post-traumatic stress disorder and fibromyalgia. She is a current smoker (4–5 cigarettes a day) but denies alcohol consumption or intravenous drug use. Her medications include ondansetron 8 mg by mouth three times a day, sertraline 50 mg by mouth twice a day and tramadol 50 mg per mouth as needed for pain.
On physical examination, her temperature was 97.9°F, her heart rate was 70 beats per minute, blood pressure 148/88 mmHg, respiration rate of 20 breaths per minute, her body mass index was 28.6 kg/m2. She was alert and oriented, but in clear distress from abdominal discomfort, rocking back and forth in bed and moaning from this pain. Her heart and lungs were clear. Her abdominal examination demonstrated no abdominal distension and no rigidity. She was tender to palpation on the right lower quadrant.
Serology analysis showed a white blood cell count of 7.7 K/μL (normal = 4–11 K/μL), Hemoglobin of 12.7 g/dL (normal = 11.5–15.3), hematocrit of 38.5% (normal = 34–45%) and platelets of 334 K/μL (normal = 140–400 K/μL). Electrolytes were all normal, and creatinine was 0.91 mg/dL (normal = 0.50–1.10 mg/dL). Lactic acid levels were 2.1 mmol/L (normal = 0.5–2.2 mmol/L). Her modified Alvarado score was four.
Computed tomography (CT) imaging showed an appendix with an appendicolith with mild dilation (9 mm) and no peri-appendiceal inflammatory changes (Fig. 1). Compared to a CT scan obtained in 2013, this study showed an appendicolith with mild dilation.
Given these findings, she was taken to the operating room for a laparoscopic appendectomy. Exploratory laparoscopy demonstrated no evidence of acute or chronic appendicitis. Pathological examination of the appendix demonstrated an appendix entirely occupied by a fecalith and no evidence of appendicitis (Fig. 2).
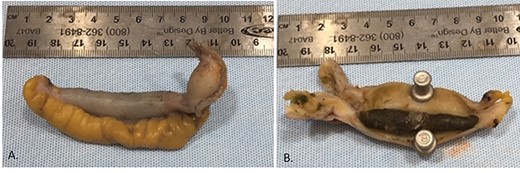
Appendiceal specimen received by pathology (A). There is a 5.0 × 0.8-cm tan/dark green fecalith filled within the lumen of the appendix (B).
CASE SERIES
Of 257 patients who were operated on for acute appendicitis at the VA North Texas Health Care System from 2005 to 2017 only 40 had fecaliths (15.6%) [Renteria and Huerta, 2018]. Of 257 patients who underwent an appendectomy initially for acute appendicitis, 38 (14.8%) had gangrenous appendicitis. Of patients with gangrenous appendicitis seven (18.4%) had an appendicolith. Fifty-three (20.6%) had a perforated appendix despite carrying an initial diagnosis of acute appendicitis. Of patients with perforated appendicitis, 11 (20.8%) had a fecalith.
REVIEW OF THE LITERATURE
Between 1939 and 2019 a total of 25 series, inclusive of 94,592 patients, were reviewed. The average age of patients was reported in 11 studies (38.2 years old ±13.3 standard deviation [SD]). The overall fecalith in appendiceal specimens was 20.7% (range 1.4–67.0%). Fecaliths occurred with a frequency of 20.3% (range 5.3–100%) in 11 reports documenting a normal appendix. Fifteen studies reported an average of 23.5% (range 1.5–65.1%) fecaliths in patients with acute appendicitis. In patients with perforated appendicitis, fecaliths were reported in 24.9% (range 10.2–39.1%) of 10 reported series (Table 1).
Frequency of fecaliths in the appendix, overall, a normal appendix, acute appendicitis and perforated appendicitis
| Year . | Number of patients . | Average age . | Overall fecalith (%) . | Fecalith in normal appendix (%) . | Fecalith in acute appendicitis (%) . | Fecalith in perforated appendicitis (%) . | Reference (PMID) . |
|---|---|---|---|---|---|---|---|
| 1939 | 372 | NR | 67.0 | NR | NR | NR | Bowers et al. [12] |
| 1943 | 91 | NR | 33.0 | NR | NR | NR | Steinert et al. [13] |
| 1963 | 71000 | NR | 44.3 | NR | NR | NR | Collins et al. [14] |
| 1965 | 240 | NR | 33.0 | NR | NR | NR | Shaw et al. [15] |
| 1979 | 55 | NR | NR | 40.0 | NR | NR | Burkitt et al. [16] |
| 1981 | 276 | NR | 16.7 | 13.0 | 45.7 | 39.1 | Butler et al. [17] |
| 1981 | 3003 | NR | 3.6 | 5.3 | 6.3 | NR | Chang et al. [18] |
| 1985 | 13 | 25 | 23.0 | NR | NR | NR | Jones et al. [9] |
| 1985 | 63 | 23 | 52.0 | NR | NR | NR | Jones et al. [9] |
| 1990 | 101 | NR | NR | 26.7 | NR | NR | Andreou et al. [19] |
| 1990 | 3124 | NR | 3.2 | NR | NR | NR | Andreou et al. [19] |
| 1990 | 405 | NR | 6.3 | NR | NR | NR | Babekir et al. [20] |
| 2006 | 200 | NR | 54.0 | NR | 26.0 | 28.0 | Herscu et al. [21] |
| 2006 | 2660 | NR | 3.7 | 6.3 | 3.5 | NR | Marudanayagam et al. [22] |
| 2008 | 427 | 24.4 | 1.4 | NR | NR | NR | Sgourakis et al. [23] |
| 2010 | 518 | 30.9 | 1.5 | NR | 1.5 | NR | Makaju et al. [24] |
| 2012 | 723 | 29.3 | 36.1 | 44.8 | 7.3 | 11.5 | Engin et al. [25] |
| 2012 | 4670 | NR | 3.6 | 60.5 | 39.5 | NR | Chandrasegaram et al. [26] |
| 2013 | 722 | NR | 13.7 | 31.6 | 12.0 | 27.5 | Singh et al. [4] |
| 2014 | 1357 | 32 | 13.7 | 34.6 | 65.1 | 10.2 | Ramdass et al. [27] |
| 2014 | 339 | 40.8 | 23.3 | NR | 63.2 | 36.7 | Kim et al. [28] |
| 2015 | 150 | NR | 13.3 | NR | 11.8 | 17.5 | Iqbal et al. [29] |
| 2017 | 225 | 69.4 | 5.8 | NR | 10.4 | NR | Khan et al. [5] |
| 2017 | 111 | 38 | NR | 100.0 | NR | NR | Khan et al. [5] |
| 2018 | 257 | 45.4 | 15.6 | NR | NR | 20.6 | Renteria et al. [8] |
| 2019 | 1007 | 38.4 | 11.1 | NR | 8.9 | 21.7 | Westfall et al. [30] |
| 2019 | 445 | 54.5 | NR | NR | 18.0 | 36.0 | Kulvatunyou et al. [31] |
| 2019 | 2038 | 44.9 | 8.0 | 6.8 | 33.0 | NR | Moskowitz et al. [32] |
| Total | 94592 | 38.2 ± 13.3a | 20.3 | 33.6 | 23.5 | 24.9 |
| Year . | Number of patients . | Average age . | Overall fecalith (%) . | Fecalith in normal appendix (%) . | Fecalith in acute appendicitis (%) . | Fecalith in perforated appendicitis (%) . | Reference (PMID) . |
|---|---|---|---|---|---|---|---|
| 1939 | 372 | NR | 67.0 | NR | NR | NR | Bowers et al. [12] |
| 1943 | 91 | NR | 33.0 | NR | NR | NR | Steinert et al. [13] |
| 1963 | 71000 | NR | 44.3 | NR | NR | NR | Collins et al. [14] |
| 1965 | 240 | NR | 33.0 | NR | NR | NR | Shaw et al. [15] |
| 1979 | 55 | NR | NR | 40.0 | NR | NR | Burkitt et al. [16] |
| 1981 | 276 | NR | 16.7 | 13.0 | 45.7 | 39.1 | Butler et al. [17] |
| 1981 | 3003 | NR | 3.6 | 5.3 | 6.3 | NR | Chang et al. [18] |
| 1985 | 13 | 25 | 23.0 | NR | NR | NR | Jones et al. [9] |
| 1985 | 63 | 23 | 52.0 | NR | NR | NR | Jones et al. [9] |
| 1990 | 101 | NR | NR | 26.7 | NR | NR | Andreou et al. [19] |
| 1990 | 3124 | NR | 3.2 | NR | NR | NR | Andreou et al. [19] |
| 1990 | 405 | NR | 6.3 | NR | NR | NR | Babekir et al. [20] |
| 2006 | 200 | NR | 54.0 | NR | 26.0 | 28.0 | Herscu et al. [21] |
| 2006 | 2660 | NR | 3.7 | 6.3 | 3.5 | NR | Marudanayagam et al. [22] |
| 2008 | 427 | 24.4 | 1.4 | NR | NR | NR | Sgourakis et al. [23] |
| 2010 | 518 | 30.9 | 1.5 | NR | 1.5 | NR | Makaju et al. [24] |
| 2012 | 723 | 29.3 | 36.1 | 44.8 | 7.3 | 11.5 | Engin et al. [25] |
| 2012 | 4670 | NR | 3.6 | 60.5 | 39.5 | NR | Chandrasegaram et al. [26] |
| 2013 | 722 | NR | 13.7 | 31.6 | 12.0 | 27.5 | Singh et al. [4] |
| 2014 | 1357 | 32 | 13.7 | 34.6 | 65.1 | 10.2 | Ramdass et al. [27] |
| 2014 | 339 | 40.8 | 23.3 | NR | 63.2 | 36.7 | Kim et al. [28] |
| 2015 | 150 | NR | 13.3 | NR | 11.8 | 17.5 | Iqbal et al. [29] |
| 2017 | 225 | 69.4 | 5.8 | NR | 10.4 | NR | Khan et al. [5] |
| 2017 | 111 | 38 | NR | 100.0 | NR | NR | Khan et al. [5] |
| 2018 | 257 | 45.4 | 15.6 | NR | NR | 20.6 | Renteria et al. [8] |
| 2019 | 1007 | 38.4 | 11.1 | NR | 8.9 | 21.7 | Westfall et al. [30] |
| 2019 | 445 | 54.5 | NR | NR | 18.0 | 36.0 | Kulvatunyou et al. [31] |
| 2019 | 2038 | 44.9 | 8.0 | 6.8 | 33.0 | NR | Moskowitz et al. [32] |
| Total | 94592 | 38.2 ± 13.3a | 20.3 | 33.6 | 23.5 | 24.9 |
aAverage age ± SD. NR, not reported.
Frequency of fecaliths in the appendix, overall, a normal appendix, acute appendicitis and perforated appendicitis
| Year . | Number of patients . | Average age . | Overall fecalith (%) . | Fecalith in normal appendix (%) . | Fecalith in acute appendicitis (%) . | Fecalith in perforated appendicitis (%) . | Reference (PMID) . |
|---|---|---|---|---|---|---|---|
| 1939 | 372 | NR | 67.0 | NR | NR | NR | Bowers et al. [12] |
| 1943 | 91 | NR | 33.0 | NR | NR | NR | Steinert et al. [13] |
| 1963 | 71000 | NR | 44.3 | NR | NR | NR | Collins et al. [14] |
| 1965 | 240 | NR | 33.0 | NR | NR | NR | Shaw et al. [15] |
| 1979 | 55 | NR | NR | 40.0 | NR | NR | Burkitt et al. [16] |
| 1981 | 276 | NR | 16.7 | 13.0 | 45.7 | 39.1 | Butler et al. [17] |
| 1981 | 3003 | NR | 3.6 | 5.3 | 6.3 | NR | Chang et al. [18] |
| 1985 | 13 | 25 | 23.0 | NR | NR | NR | Jones et al. [9] |
| 1985 | 63 | 23 | 52.0 | NR | NR | NR | Jones et al. [9] |
| 1990 | 101 | NR | NR | 26.7 | NR | NR | Andreou et al. [19] |
| 1990 | 3124 | NR | 3.2 | NR | NR | NR | Andreou et al. [19] |
| 1990 | 405 | NR | 6.3 | NR | NR | NR | Babekir et al. [20] |
| 2006 | 200 | NR | 54.0 | NR | 26.0 | 28.0 | Herscu et al. [21] |
| 2006 | 2660 | NR | 3.7 | 6.3 | 3.5 | NR | Marudanayagam et al. [22] |
| 2008 | 427 | 24.4 | 1.4 | NR | NR | NR | Sgourakis et al. [23] |
| 2010 | 518 | 30.9 | 1.5 | NR | 1.5 | NR | Makaju et al. [24] |
| 2012 | 723 | 29.3 | 36.1 | 44.8 | 7.3 | 11.5 | Engin et al. [25] |
| 2012 | 4670 | NR | 3.6 | 60.5 | 39.5 | NR | Chandrasegaram et al. [26] |
| 2013 | 722 | NR | 13.7 | 31.6 | 12.0 | 27.5 | Singh et al. [4] |
| 2014 | 1357 | 32 | 13.7 | 34.6 | 65.1 | 10.2 | Ramdass et al. [27] |
| 2014 | 339 | 40.8 | 23.3 | NR | 63.2 | 36.7 | Kim et al. [28] |
| 2015 | 150 | NR | 13.3 | NR | 11.8 | 17.5 | Iqbal et al. [29] |
| 2017 | 225 | 69.4 | 5.8 | NR | 10.4 | NR | Khan et al. [5] |
| 2017 | 111 | 38 | NR | 100.0 | NR | NR | Khan et al. [5] |
| 2018 | 257 | 45.4 | 15.6 | NR | NR | 20.6 | Renteria et al. [8] |
| 2019 | 1007 | 38.4 | 11.1 | NR | 8.9 | 21.7 | Westfall et al. [30] |
| 2019 | 445 | 54.5 | NR | NR | 18.0 | 36.0 | Kulvatunyou et al. [31] |
| 2019 | 2038 | 44.9 | 8.0 | 6.8 | 33.0 | NR | Moskowitz et al. [32] |
| Total | 94592 | 38.2 ± 13.3a | 20.3 | 33.6 | 23.5 | 24.9 |
| Year . | Number of patients . | Average age . | Overall fecalith (%) . | Fecalith in normal appendix (%) . | Fecalith in acute appendicitis (%) . | Fecalith in perforated appendicitis (%) . | Reference (PMID) . |
|---|---|---|---|---|---|---|---|
| 1939 | 372 | NR | 67.0 | NR | NR | NR | Bowers et al. [12] |
| 1943 | 91 | NR | 33.0 | NR | NR | NR | Steinert et al. [13] |
| 1963 | 71000 | NR | 44.3 | NR | NR | NR | Collins et al. [14] |
| 1965 | 240 | NR | 33.0 | NR | NR | NR | Shaw et al. [15] |
| 1979 | 55 | NR | NR | 40.0 | NR | NR | Burkitt et al. [16] |
| 1981 | 276 | NR | 16.7 | 13.0 | 45.7 | 39.1 | Butler et al. [17] |
| 1981 | 3003 | NR | 3.6 | 5.3 | 6.3 | NR | Chang et al. [18] |
| 1985 | 13 | 25 | 23.0 | NR | NR | NR | Jones et al. [9] |
| 1985 | 63 | 23 | 52.0 | NR | NR | NR | Jones et al. [9] |
| 1990 | 101 | NR | NR | 26.7 | NR | NR | Andreou et al. [19] |
| 1990 | 3124 | NR | 3.2 | NR | NR | NR | Andreou et al. [19] |
| 1990 | 405 | NR | 6.3 | NR | NR | NR | Babekir et al. [20] |
| 2006 | 200 | NR | 54.0 | NR | 26.0 | 28.0 | Herscu et al. [21] |
| 2006 | 2660 | NR | 3.7 | 6.3 | 3.5 | NR | Marudanayagam et al. [22] |
| 2008 | 427 | 24.4 | 1.4 | NR | NR | NR | Sgourakis et al. [23] |
| 2010 | 518 | 30.9 | 1.5 | NR | 1.5 | NR | Makaju et al. [24] |
| 2012 | 723 | 29.3 | 36.1 | 44.8 | 7.3 | 11.5 | Engin et al. [25] |
| 2012 | 4670 | NR | 3.6 | 60.5 | 39.5 | NR | Chandrasegaram et al. [26] |
| 2013 | 722 | NR | 13.7 | 31.6 | 12.0 | 27.5 | Singh et al. [4] |
| 2014 | 1357 | 32 | 13.7 | 34.6 | 65.1 | 10.2 | Ramdass et al. [27] |
| 2014 | 339 | 40.8 | 23.3 | NR | 63.2 | 36.7 | Kim et al. [28] |
| 2015 | 150 | NR | 13.3 | NR | 11.8 | 17.5 | Iqbal et al. [29] |
| 2017 | 225 | 69.4 | 5.8 | NR | 10.4 | NR | Khan et al. [5] |
| 2017 | 111 | 38 | NR | 100.0 | NR | NR | Khan et al. [5] |
| 2018 | 257 | 45.4 | 15.6 | NR | NR | 20.6 | Renteria et al. [8] |
| 2019 | 1007 | 38.4 | 11.1 | NR | 8.9 | 21.7 | Westfall et al. [30] |
| 2019 | 445 | 54.5 | NR | NR | 18.0 | 36.0 | Kulvatunyou et al. [31] |
| 2019 | 2038 | 44.9 | 8.0 | 6.8 | 33.0 | NR | Moskowitz et al. [32] |
| Total | 94592 | 38.2 ± 13.3a | 20.3 | 33.6 | 23.5 | 24.9 |
aAverage age ± SD. NR, not reported.
DISCUSSION
A fecalith (also known as stercolith, coprolith, appendicolith or concretion) is a fecal concretion or pellet occupying the appendiceal lumen and is thought to be the result of a low fiber diet that accompanies a Western society lifestyle [11]. Popularized by early findings of giant surgeons [2] and propagated by animal studies showing appendicitis after appendiceal obstruction in rabbits [12], current surgical textbooks support the role of a fecalith as a major cause of appendicitis in adults [1].
The present analysis was stimulated by an unusual case in which a patient presented with a history of abdominal pain and had a large fecalith within the entire lumen of the appendix but did not cause appendicitis. A review of 257 veteran patients who had undergone an appendectomy for acute appendicitis at our institution, only 15.6% had fecaliths on the pathological specimen. A review of the literature showed that less than a quarter of patients presenting with appendicitis demonstrated a fecalith either radiographically, in the operating room, or on final pathology examination (Table 1).
The present case negates the role of the fecalith in the infectious process of appendicitis, even if it is very large. Our case series consists of veteran patients presenting with acute appendicitis and shows that fecaliths are found rarely in this patient population. The literature review demonstrated the following findings: (i) There is a wide range in the incidence of fecaliths leading to appendicitis; (ii) more cases of a normal appendix have been documented that have incidental fecaliths within the lumen compared to the frequency of a fecalith causing appendicitis; (iii) A temporal variation in the incidence of fecaliths as a cause of acute appendicitis has been proposed by Sigh et al. that divides this era prior to the 1970s and after that to current studies [4] and (iv) overall, there is an association between fecaliths and a risk of perforated appendicitis.
A fecalith is, therefore, an infrequent cause of appendicitis as suggested by textbooks. Other causes of appendicitis have been proposed and reviewed by Norman J Carr [13] and include appendiceal ulceration leading to infection, hygiene (enteric infection as a result of exposure of environmental factors), diet (appendicitis is less common in developing countries), ischemia, trauma, genetics, foreign bodies and type I hypersensitivity, and increased contractability of the appendix [13].
Thus, the current literature argues against a fecalith leading to acute appendicitis, but when present it is more likely to lead to perforation. This should be considered when assessing a patient for NOM of early appendicitis.
CONFLICT OF INTEREST STATEMENT
None of the authors have any conflicts of interest to disclose.
FUNDING
None.



