-
PDF
- Split View
-
Views
-
Cite
Cite
James E Archer, Adrian Gardner, A case of missed unstable cervical injury during the COVID-19 pandemic, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa293, https://doi.org/10.1093/jscr/rjaa293
Close - Share Icon Share
Abstract
This case report discusses a patient with a significant, unstable, three-column injury of the cervical spine, which was not initially detected and was subsequently found on reassessment at 2 weeks post injury. The report discusses the imaging findings and the subsequent management of the injury. The report highlights the need for an individualized assessment of each presentation, taking into account the circumstances of injury and any pre-existing degenerative change in the spine.
INTRODUCTION
This case report describes a case of missed, unstable, three-column injury of the cervical spine after a road traffic collision in an elderly patient during the coronavirus disease 2019 (COVID-19) pandemic. The mechanism of distractive flexion through a stiff, degenerate spine is discussed along with the management of this injury. The need for an individualized assessment after any trauma to include an understanding of the circumstances of injury, a physical examination and imaging studies, including both computer tomography (CT) and magnetic resonance imaging (MRI) is highlighted.
CASE REPORT
A 76-year-old lady was involved in a road traffic collision, after being dazzled by the sun, where she crashed into a parked vehicle and rolled her car twice. She was taken to her nearest emergency department and assessed following advanced trauma life support protocols. She was haemodynamically normal and had no neurological deficit. She complained of neck and left shoulder pain. Due to the mechanism of her injury and her complaint of neck pain, a CT scan of her cervical spine was performed along with an x-ray of her left shoulder.
The left shoulder radiograph showed no abnormality. The sagittal images of the cervical spine CT scan are shown in Figs 1 and 2a and b. Figure 1 is the mid-sagittal slice of the CT scan at presentation and shows no obvious malalignment.
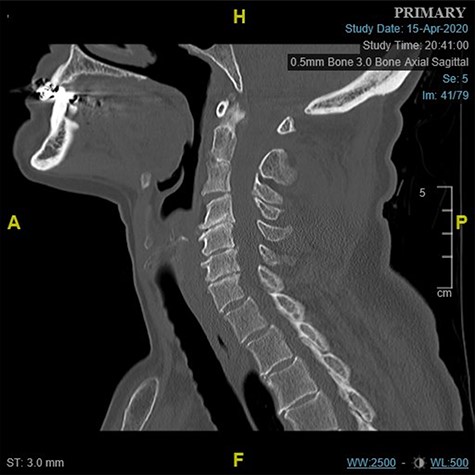
Midline sagittal CT scan of the cervical at the time of first presentation.
There is an acute fracture of the antero-superior osteophyte of the body of C7 (Fig. 2a). There is also opening of the cervical facet at C6/7 (Fig. 2b). There were no fractures of the vertebral bodies. It can also be appreciated that there is significant degenerative change between C4 and C7.
On the basis of these imaging findings, the patient was reassured that no injury had been identified. Due to the COVID-19 pandemic, the patient was discharged home after this and no further follow up was arranged to ensure that both the patient and the hospital were protected from additional risk associated with COVID-19.
Two weeks later the patient was reviewed at home by her general practitioner due to ongoing neck pain, left shoulder pain and subjective numbness and weakness in her left arm. Upon assessment, it was noted that she held her neck in a flexed position and was unable to straighten the neck. The general practitioner arranged for an urgent review by the orthopaedic team in the nearest hospital. On assessment they recognized the potential for a significant injury and arranged an x-ray and a MRI of the cervical spine. Fig. 3 shows the lateral cervical spine radiograph demonstrating an anterior subluxation of the C6 vertebrae on C7 and significant malalignment between the spinous processes of C6 and C7.
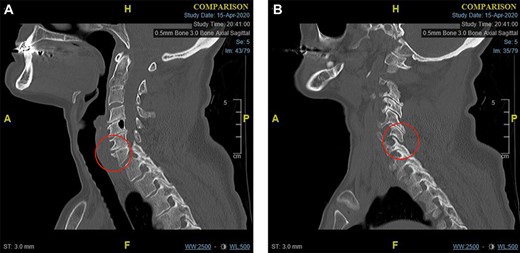
(a) Para-midline sagittal CT scan of the cervical spine at the time of first presentation showing a fracture of the antero-superior osteophyte of C7 (indicated with a circle). and (b) Para-midline sagittal CT scan of the cervical spine at the time of first presentation showing opening of the C6/C7 facet joint (indicated with a circle).
The MRI scan shows that the dislocation had reduced. Fig. 4a demonstrates high signal in the C6/C7 intervertebral disc.
Fig. 4b also demonstrates the injury to the posterior ligament complex at C4 to C7.
The case was discussed with the regional spinal surgery unit and subsequently urgently transferred. The case represented a missed unstable cervical spinal injury. Stabilization of the injury was performed with a two-stage procedure. First, an anterior

Lateral cervical spine radiograph at the time of representation with the level of injury indicated.
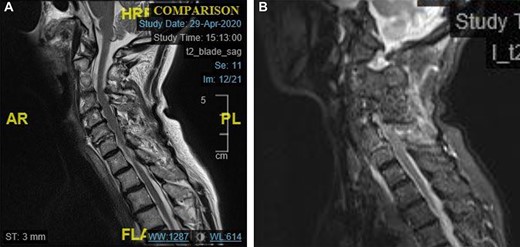
(a) Midline sagittal T2 weighted MRI image showing high signal in the C6/7 disc space. (b) Midline sagittal short-t1 inversion recovery weighted MRI image showing high signal in the posterior elements of C4–C7.
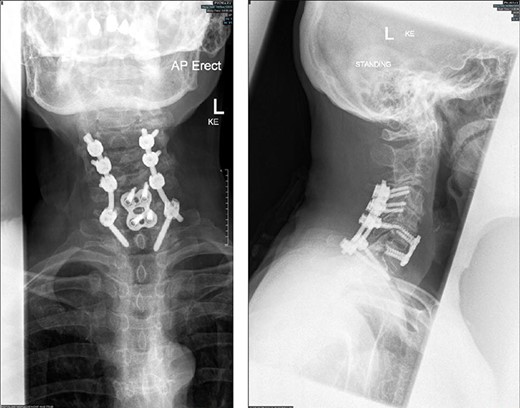
Radiographs (antero-posterior and lateral views) of the cervical spine following instrumentation.
approach was performed to reconstruct the anterior column using an anterior cervical discectomy and fusion through the C6/7 disc space. This was performed with a CeSPACE cage (B Braun, Hessen, Germany) and a Venture anterior cervical locking plate (Medtronic, Minneapolis, MN, USA). The patient was then turned prone and a posterior approach to the spine was performed. An instrumented fusion was performed using lateral mass screws in C4, C5 and C6 and pedicle screws in T1 bilaterally using Mountaineer (Depuy Synthes, Raynham, MA, USA). Grafton bone graft substitute (Medtronic, Minneapolis, MN, USA) was used in both the anterior and posterior stages.
She made a good post-operative recovery, and the upper limb neurological symptoms resolved. Post-operative radiographs are shown in Fig. 5.
DISCUSSION
The mechanism of this injury is best described as distractive flexion [1]. This mechanism describes the head moving into flexion and away from the trunk such that tension forces are applied to the posterior elements of the spine. The soft tissue sequentially fails from posterior to anterior and results in facetal dislocation. This injury is highly unstable and is associated with neurological injury [2] and even devastating paralysis [3, 4]. In this case, the dislocation reduced when lying supine when undergoing the CT scan and was not appreciated.
Whilst the BOAST guidance for spinal clearance in the trauma patient [5] recommends modern helical CT scanning, it is apparent that there is also use of MRI to clear the spine in the presence of a normal CT scan in the UK [6].
In this case, the subaxial degenerative change has acted in a similar fashion to that seen in ankylosing disorders, with a transverse three-column injury though a disc space surrounded by relatively stiff segments of the spine [7]. In ankylosing disorders, it is recognized that fractures are difficult to diagnose and a low threshold for the use of MRI is indicated [8] and that MRI scanning generally has an important role in suspected ligamentous injury [9].
This case highlights the importance of a high index of suspicion for a significant cervical spine injury in the presence of a stiff and degenerate cervical spine, even in the presence of minimal and subtle changes on a CT scan. This, combined with a high-energy mechanism, and significant neck pain, requires further assessment and imaging after a CT scan. The discharge of this elderly patient from the emergency department was likely to have been heavily influenced by the COVID-19 pandemic and the desire to manage any patients non-operatively or in a non-hospital setting where possible.
However, even when such challenges present, ensuring high-quality patient care is essential. As highlighted by the imaging performed at her reassessment, the facet dislocation may spontaneously reduce making diagnosis more challenging. This case highlights the need for clinical assessment and vigilance for potentially hidden injuries.
CONFLICT OF INTEREST STATEMENT
None declared.



