-
PDF
- Split View
-
Views
-
Cite
Cite
Guillaume Tcheutchoua Soh, Papa Mamadou Faye, Heritier Molengo Emeki, Coumba Diagne, Ousmane Thiam, Alpha Oumar Toure, Mamadou Cisse, Ascaris lumbricoides infestation of the gallbladder: case report, Journal of Surgical Case Reports, Volume 2025, Issue 12, December 2025, rjaf975, https://doi.org/10.1093/jscr/rjaf975
Close - Share Icon Share
Abstract
A 41-year-old woman presented with 3 days of right hypochondria and epigastric pain with vomiting. Laboratory results showed 4730 white blood cells, with eosinophils at 1.3% and C-reactive protein of 7.23 mg/L. We suspected hepatic colic. Ultrasonography revealed a long, floating, zigzagging tubular structure in the gallbladder, indicating the presence of a live worm. We concluded that the gallbladder was infested with Ascaris lumbricoides. The patient was treated with albendazole, leading to clinical improvement, and she was advised on prevention. Gallbladder infestation is a hepatobiliary complication of ascariasis. The worm appears as a mobile, zigzagging tubular structure within the gallbladder, resembling a “swimmer in the gallbladder.” This appearance is easily recognizable on ultrasound and has been reported in cases of live Ascaris. In uncomplicated cases, antihelminthics may suffice. Monitoring is necessary because taking antiparasitic drugs can precipitate the onset of complications by retaining dead worms in the bile duct.
Introduction
Intestinal ascariasis is a widespread parasitic disease with a particularly high prevalence in areas with low socioeconomic status and poor hygiene [1]. This parasite is unique in that it can cause surgical complications in the digestive tract [2–5]. Intestinal obstruction is the most common complication of intestinal ascariasis [6]. Rarely, Ascaris can enter the bile ducts and lead to complications such as pancreatitis, hepatic colic, cholangitis, biliary peritonitis, or precipitate the formation of stones [5, 7–10]. These complications pose specific diagnostic and therapeutic challenges. Abdominal ultrasound, abdominal CT, MRI, and endoscopy play a role in the presumptive diagnosis, which is confirmed by species identification by biologists [7]. Treatment may involve antiparasitic therapy or surgical techniques, such as cholecystectomy, exploration of the common bile duct and placement of a T-tube drain, or advanced endoscopic techniques such as endoscopic retrograde cholangiopancreatography with or without sphincterotomy [7]. The results are unpredictable, as they can be simple or lead to serious complications such as biliary peritonitis. This article reports a case of Ascaris infection of the gallbladder with a didactic video to raise awareness and recognition of this condition by radiologists and clinicians. This study was reported in accordance with the CARE guidelines [11].
Case report
A 41-year-old woman with no significant medical history presented to the emergency department with abdominal pain marked in the right hypochondrium and epigastrium. This was associated with four episodes of postprandial vomiting of 3-day duration. Physical examination revealed tenderness in the epigastric and right hypochondrium regions. She was admitted and underwent an abdominal ultrasound, which revealed acute cholecystitis with vesicular sludge as a notable sign. Blood tests showed mild hypokalemia (3.1 mmol/L), C-reactive protein at 7.23 mg/L, and a white blood cell count of 4730 with an eosinophil count of 1.3% of white blood cells. We suspected hepatic colic. Since no biological disorder was identified, we had a second radiologist perform an ultrasound, which allowed us to visualize a floating and zigzagging central anechoic tube that lacked shadowing in the gallbladder with no signs of cholecystitis (Fig. 1 and Video SS1). This finding is consistent with the presence of worms swimming inside the gallbladder. We completed our history with the patient, who admitted that she did not take deworming medication regularly. She also admitted to having episodes of nocturnal cough 2 weeks earlier, which had improved without treatment. This finding was suggestive of Loffler’s syndrome. We concluded that the patient had vesicular Ascaris lumbricoides. The stool test was not available in emergencies or at weekends. The patient was treated with 400 mg of albendazole and amoxicillin combined with clavulanic acid and was monitored for 3 days in the hospital. The outcome was favorable, and the patient was followed up over a month with no recurrence and ultrasound was normal. She was advised on preventive and hygienic measures.
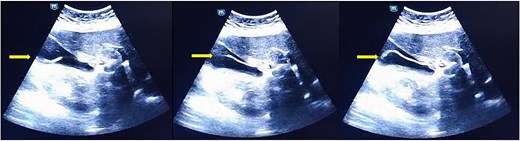
Floating and zigzagging central anechoic tube which lack of shadowing into the gallbladder.
Discussion
Gallbladder infestation is a rare hepatobiliary complication of intestinal ascariasis due to narrowing of the cystic duct [12]. The prevalence of this condition has decreased due to the prophylactic treatment of worms [13]. In low-income countries and poor sanitation areas, gastrointestinal complication of Ascaris infection is still observed and reported [2, 6, 12]. There is also poor adherence to prophylactic treatment, as seen in our patient. Gallbladder infestation poses a diagnostic challenge for both clinicians and radiologists [9]. The case of gastrointestinal ascariasis we present was free and alive in the gallbladder, giving the appearance of a mobile zigzagging tubular structure within the gallbladder, like a “swimmer in the gallbladder.” This appearance is easily recognizable on abdominal B-mode ultrasound and has also been reported by Khanduri in cases of live Ascaris [14]. The main differential diagnosis on ultrasound is the presence of vesicular sludge. In our case, the first ultrasound concluded this, and there was doubt in front of clinical, biological, and imaging discordance. A high level of suspicion is required to diagnose this condition. Examination of the specimen was not possible. Another diagnostic test is the ELISA test, which can detect recent contact with the parasite. However, due to its cost, it is not available in our center or in low-income areas [15]. Other signs were searched, such as the presence of Loffler’s syndrome, which is characterized by a high eosinophilic count and transient radiological infiltration observed on chest X-ray associated with cough. This can be observed during the parasitic cycle of Ascaris [1, 16]. In our case, the patient reported respiratory symptoms 2 weeks earlier, which improved without treatment.
In the absence of complications such as obstruction or perforation, as in our case, medical treatment with benzimidazoles may be sufficient [1, 10]. Monitoring is necessary because the presence of other adult worms in other orifices cannot be ruled out, and taking antiparasitic medication may precipitate the onset of complications by causing the death of the parasite in the cystic duct [1, 2]. In our case, monitoring lasted for 3 days. The main tool for preventing this disorder is the administration of antiparasitic drugs and reinforcement of sanitary measures. This advice was given to the patient.
The key message of this case is that gallbladder Ascaris infestation can present a particular aspect on ultrasound when the worm is alive; its visualization is rare but is easily detected on ultrasound. It has become rare because of public health preventive measures. Poor sanitation and low adherence to these measures led to the persistence of rare cases. Young radiologists and clinicians may pay attention to identifying their appearance on ultrasound, especially those who work in low-income settings.
Conclusion
Gallbladder infestation by Ascaris lumbricoides is rare due to cystic duct narrowing. Ultrasound makes it easy to diagnose when the worm is alive, as it appears as a tubular structure that swims freely in the gallbladder. When species identification is not possible, other signs of ascariasis can help with diagnosis. In the absence of complications, medical treatment is sufficient but requires careful monitoring.
Acknowledgements
We thank Josiane Ngouanfo Tchoffo for her support when editing the files in English.
Author contributions
Conception and study design: Guillaume Tcheutchoua Soh, Papa Mamadou Faye. Drafting of the article: Guillaume Tcheutchoua Soh, Papa Mamadou Faye, Héritier Molengo Emeki, and Coumba Diagne. Final approval: Ousmane Thiam, Alpha Oumar Toure, and Mamadou Cisse.
Conflict of interest statement
None declared.
Funding
The authors declare they have received no funding for the preparation of this document.



