-
PDF
- Split View
-
Views
-
Cite
Cite
David Bellido-Yarlequé, Kelly Meza, José Palacios, Jorge Cervera, Fernando Anicama, Giant benign teratoma occupying the left hemithorax with pleural effusion: a rare presentation, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa294, https://doi.org/10.1093/jscr/rjaa294
Close - Share Icon Share
Abstract
Mature teratomas are the third most common mediastinal tumors. Giant teratoma in pediatric population is rare. A resection of giant benign teratoma in left hemithorax was performed in a 4-year-old patient. The computed tomography scan showed the presence of a large multiloculated mediastinal mass extending to the left pleural space and pleural effusion. The patient underwent total resection of the mediastinal mass via a median sternotomy associated to left anterior thoracotomy. Entry into the pleural space was performed through the sixth intercostal space to obtain safe visualization of the cavity and proceed to tumor excision. The collapsed left lung was re-expanded, and the patient was extubated. Despite the size and the surrounding structures of the teratoma, our preoperative preparation and surgical technique were effective and resulted in favorable recovery without complications and a posterior normal left lung function.
INTRODUCTION
Mature teratomas are the third most common mediastinal tumor [1]. It is more frequent in patients around their second and third decades of life. Although most cases are reported as slow-growing tumors, rapid growth symptomatic mediastinal teratomas are unusual. Due to potential risk of rupture and infection, immediate surgical resection is recommended [2]. Presented in this report, we describe a case of giant mature teratoma that grew rapidly and required prompt resection in a pediatric patient.
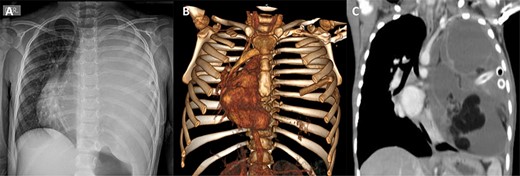
(A) Preoperative chest X-ray showing total atelectasis of the left lung and deviation of the cardiac silhouette to the right. (B) CT scan showing deviation of the cardiac silhouette to the right. (C) Heterogenic density tumor multiloculated of the left hemithorax, which probably originated in the mediastinum and extended to the whole left pleural space with displacement of the mediastinum to the right
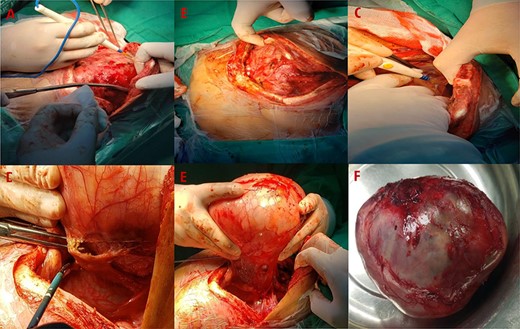
(A) Resection of the mediastinal mass via a median sternotomy associated to left anterior thoracotomy. (B) Entry into the pleural space was performed through the sixth intercostal space. (C) Many adhesions to thoracic wall and diaphragm were found. (D) Phrenic nerve presented adhesions to the tumor. Also, it had founded a nutritional artery depending on left internal mammary artery. (E) Section of the left internal mammary vessels, dissection of the phrenic nerve, ligation of the nutritional vessel, mediastinal tumor excision, ligation of the thymic vessels and thymectomy was performed. (F) The mediastinal tumor, excised in block, was red–gray colored, well circumscribed and capsuled with a size of 15 × 15 × 20 cm
CASE REPORT
A 4-year-old female with complete vaccines and without prior pathological prenatal history was admitted and transferred with a diagnosis of pleural effusion from a primary health center where a thoracic drainage tube was placed. She presented a 1-month history of progressive cough, fever and dyspnea. The physical exam was relevant for thoracic asymmetry, diminished breath sounds and vocal vibrations in the left hemithorax. A chest X-ray showed a total occlusion of the left hemithorax with deviation of the mediastinum to the right side. A computed tomography (CT) scan showed pectus excavatum and the presence of a large multiloculated mediastinal mass extending to the left pleural space (Fig. 1). The mass was heterogeneous containing soft tissue elements, cystic areas and calcification. Laboratory workup was remarkable for mild anemia (hemoglobin 10.2 g/dl), eosinophilia (5.2 cells × 109/l) and elevated alkaline phosphatase. α-Fetoprotein (AFP) and β-human chorionic gonadotropin (β-hCG) were both normal; cancer antigen-125 (CA-125) was elevated (83.3 UI/ml, normal <46 U/ml). Initial assessment suggested benign teratoma.
The patient underwent a total resection of the mediastinal mass via a median sternotomy. Given the extension of the teratoma and adhesions to the chest wall, an additional approach with a left anterior thoracotomy was made (Fig. 2). Entry into the pleural space was performed through the sixth intercostal space to obtain safe visualization of the cavity and proceed to tumor excision. Many adhesions were found to the thoracic wall, diaphragm and phrenic nerve. Additionally, a nutritional artery depending on left internal mammary artery was discovered with collateral veins draining to brachiocephalic vein. A section of the left internal mammary vessels, dissection of the phrenic nerve, ligation of the nutritional vessel, mediastinal tumor excision, ligation of the thymic vessels and thymectomy was performed. Thoracic drainage tubes (two) were placed. The mediastinal tumor, excised in block, was red–gray colored, well circumscribed and capsuled with a size of 15 × 15 × 20 cm. Postoperatively, the collapsed left lung was re-expanded, and the patient was extubated on Day 1 (Fig. 3). The patient recovered from the operation and was discharged on the ninth postoperative day. Preoperative atelectasis of the left lung partially resolved, and the pathological examination revealed a benign mature teratoma with cystic degeneration. Anatomical pathology test showed the presence of glandular epithelial cells concomitant with the presence of cartilage tissue (Fig. 4) The histochemistry test revealed CD3(+) CD20(+) TDT(−) CD5(−) cells. Thymic tissue was negative for malignancy; nine lymph nodes showed reactive follicular hyperplasia.
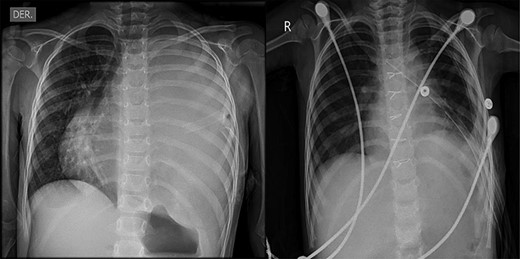
(A) Preoperative chest X-ray showing total atelectasis of the left lung and deviation of the cardiac silhouette to the right. (B) Postoperative Day 9 chest X-ray after total resection of the teratoma, showing re-expansion of the left lung
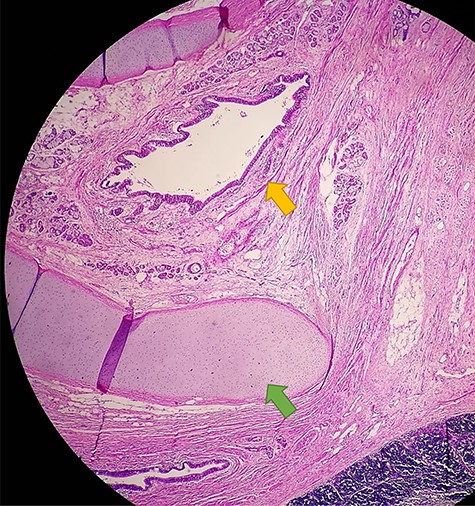
Anatomical pathology test showing the presence of glandular epithelial cells (yellow arrow) concomitant with the presence of cartilage tissue (green arrow)
DISCUSSION
Giant teratomas are defined as those that occupy more than half of a hemithorax [3]. Teratomas are slow-growing tumors with ~36–62% of cases presenting asymptomatic at the time of diagnosis [4]. However, symptoms such as chest pain, cough, dyspnea and murmur simulating a valvular heart disease can be presented due to compression of neighboring structures and when they reach a considerable size. Diaphragmatic paralysis and vocal cords paralysis have been described due to phrenic nerve and larynx nerve compression by teratoma, respectively [5]. In our patient, the appearance and growth of the teratoma was considered in an approximate period of 18 months due to a normal chest X-ray image before her hospital admission. Tumor markers such as AFP and hCG are usually within reference range in benign teratomas but may be elevated in malignant embryonic tumors [6]. Likewise, our patient had normal AFP and hCG, but abnormal serum CA-125 level, the latter likely related to inflammation of the pleura.
Rapidly growing teratoma occurs in rare cases due to the secretion of ectopic hormones and digestive enzymes from pancreatic, gastric, intestinal tissue, which through glandular secretion promotes the degradation of surrounding structures, associating them with complications such as pleural effusion, hemoptysis and thoracic pain [7]. In our patient, gastric gland and intestinal tissue were found in the histology of the tumor suggesting the above theory as a possible explanation for our patient’s clinical presentation expressed as pleural effusion and rapid growth. Due to the age of the patient, the growth rate of the tumor and pleural effusion associated, this case has a rare presentation.
Diagnostic imaging is important for the initial evaluation of teratoma. CT scan is the gold standard imaging for the evaluation of cystic and/or solid masses within the mediastinum [8]. The typical CT scan description includes a homogeneous, markedly marginalized, lobed mass with intrinsic elements such as soft tissue, fat, areas of cystic calcifications and fatty liquid [9].
Tumor resection approaches includes median sternotomy, thoracotomy and video-assisted thoracoscopic surgery. Various studies have reported lateral thoracotomy as the means of boarding in the case of tumor invasion into a hemithorax, with surgical approaches depending on tumor size, type and surrounding structures [10]. In our patient, a median sternotomy associated with left anterolateral thoracotomy was inevitable due to the size of the tumor and its occupancy in the left hemithorax. If the surgery had been performed when the teratoma had a smaller size, some minimally invasive surgical approach could have been done. Because the tumor did not compromise the left lung, at the time of exeresis of the teratoma, the left lung was re-expanded without any difficulties and a left pneumonectomy was not required improving the patient’s prognosis.
Giant teratoma in pediatric population is rare. A resection of giant benign teratoma in left hemithorax was performed in a 4-year-old patient. Despite the size and the surrounding structures of the teratoma, our preoperative preparation and surgical technique were effective and resulted in favorable recovery without complications and a posterior normal left lung function.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



