-
PDF
- Split View
-
Views
-
Cite
Cite
Yumi Muranishi, Soh Nishimoto, Kenichiro Kawai, Hisako Ishise, Masao Kakibuchi, An occult case of the first branchial cleft anomaly, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa291, https://doi.org/10.1093/jscr/rjaa291
Close - Share Icon Share
Abstract
We report a case of the first branchial cleft anomaly, clinically typical but occult in images and pathology. An 8-year-old female who had an induration below her right mandibular angle was referred to our department with a diagnosis of an infectious epidermal cyst. CT and MRI had shown no evidence of fistula or cyst. At the initial operation, a string structure was observed, but pathologically no epithelial structure was observed. However, the infection at the same site repeated and the symptoms became more severe than before. Considering a high probability of the first branchial anomaly, partial parotidectomy was performed as radical surgery. A cord structure attached to subcutaneous tissue at the intertragal notch was found. Although no epithelial component in the pathology was detected, this string structure was clinically considered as the rudimentary form of the first branchial anomaly.
INTRODUCTION
Branchial clefts can be seen in the 5-week embryo. The first branchial cleft is the groove between the first and second branchial arches. It will partly persist and form the epithelium of the external auditory canal and part of the tympanic membrane. The first branchial cleft anomaly, caused by the unusual residue of the cleft epithelium, is relatively uncommon and accounts for less than 1 to 10% of all branchial anomalies [1–3]. Here, we present a case of first branchial cleft anomaly, clinically typical but occult in images and pathology.
CASE REPORT
An 8-year-old Japanese girl was introduced to our department from an ear-nose-throat doctor, with a diagnosis of infected epidermal cyst. She had a subcutaneous induration with a diameter of 5 × 12 mm, below the right mandibular angle (Fig. 1). Recurrent inflammation had been persisting for a year. Pediatrist had followed her with a diagnosis of recurrent parotitis. Previously, CT (Fig. 2) and MRI images had been taken and the radiologist found small calcifications in her right parotid gland but no sign of parotitis, cysts or fistula. No other abnormality, including extra auricular canal, was detected. No particular family history was recorded.

An 8-year-old girl had a chronic induration below her right mandibular angle.
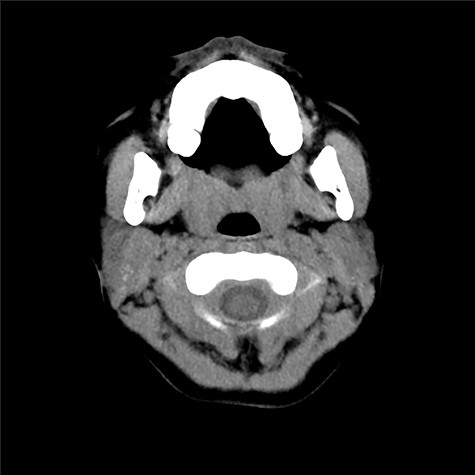
CT scan taken prior to the first visit. There can be seen subcutaneous induration, but no cysts nor fistula was obvious.
Under general anesthesia, the ablative operation was performed. Christal violet ink was used to dye inside of the cavity. Beneath the induration was observed a string structure, halfway dyed, adhering to the fascia on the sternocleidomastoid muscle (Fig. 3). With a part of the fascia, the string was pursued but could be followed no further than the frontier border of the muscle. The wound was closed primarily.

A string-like structure was observed below the induration, during the first surgery.
In the histological report, only fibrous scar was found without a sign of fistula or epithelial cells (Fig. 4).
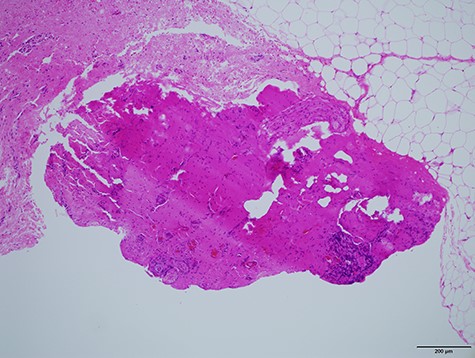
Histological specimen showing the string-like structure. No epithelial cells were observed by the pathologists.
A year after the surgery, small subcutaneous infection with pus appeared on the scar. Oral administration of antibiotics was able to control it. Though it appeared every 3–6 months, still no sign of fistula could be found by CT scan. To the parents, a high possibility of the residual first branchial cleft fistula was explained. Total resection of the fistula was suggested with a potential risk of facial nerve palsy. At this moment, they could not consent to the surgery.
Three and a half years after the initial surgery, she presented with high fever and painful swelling of her right parotid area (Fig. 5). CT scan presented swelling of the parotid gland (Fig. 6). No cystic structure could be pointed out. Under general anesthesia, incision, cleansing and drainage were done. Staphylococcus aureus was identified in the pus. Decline of fever was obtained and remission of the abscess was seen.

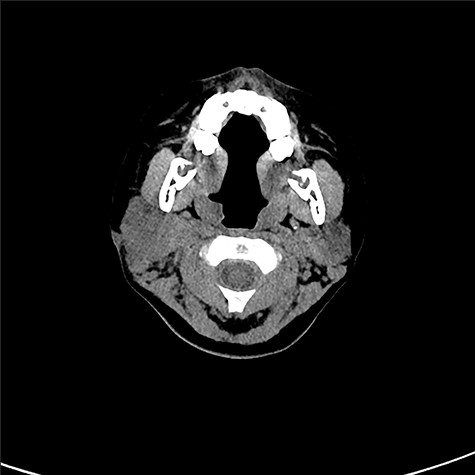
Cystic lesion could not be observed by CT scan prior to the drainage.
Total extirpation of the fistula with partial parotidectomy was suggested to the patients again. Also, the potential risk of facial nerve palsy was explained. They consented to the surgery.
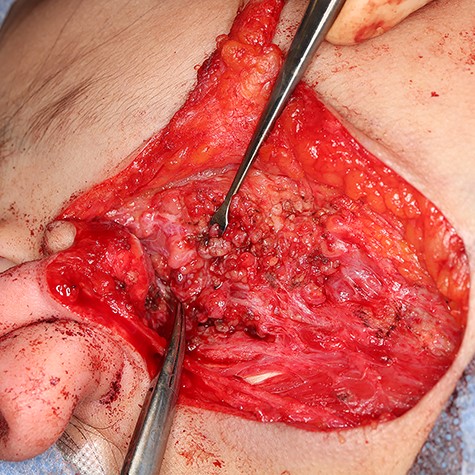
Two months after the infection, again under general anesthesia, radical surgery was done. As there remained no cystic lesion at this moment, dye could not be used. Parotidectomy incision was done and the flap was raised superficial to the parotid fascia. Great auricular nerve was identified and preserved. In the beginning, the positional relationship of the anomalous structure with the facial nerve was not known. A cord structure was found on the backside of intertragal notch (Fig. 7). It was attached to subcutaneous tissue, but no opening to the external auricular canal was confirmed. It passed into the parotid gland. Because it was difficult to divide it from the gland, partial glansectomy was done. Because of scar formation, identification of facial nerve branches inside the gland, especially in the lower part, was not easy. Tracking retromandibular vein and nerve stimulator helped us. At last, they were identified and preserved (Figs 8 and 9). The patient was discharged without facial palsy. Recurrence of the swelling has not been seen for a year, at her age of 12.
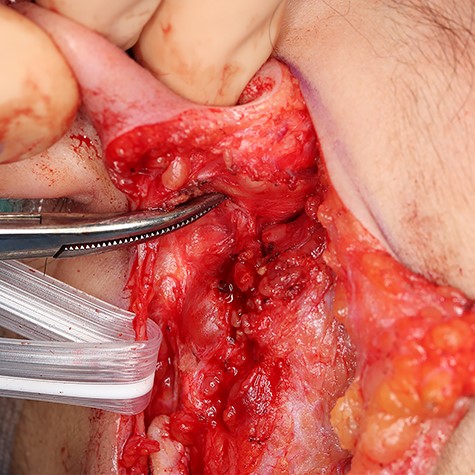
A cord structure is pointed by a mosquito clamp. Great auricular nerve was yanked with a Penrose drain.
Facial nerve branches were preserved and pointed by a mosquito clamp.

Extracted parotid gland specimen. Strings were tied to the cord structure.
Histologically (Fig. 10), fibrosis and inflammatory granulation were seen. Inflammatory reaction of lymph nodes was observed. Epithelial cells could not be found in the slices.
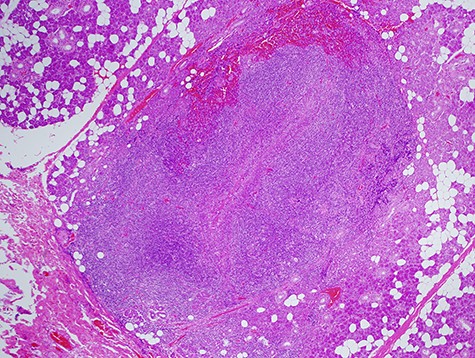
Histological specimen of the final surgery. Inflammatory reaction of a lymph node inside of parotid the parotid gland was observed.
DISCUSSION
D’Souza et al. reviewed 158 reported cases from 55 publications [3]. The incidence of facial nerve palsy was statistically higher when it was not identified during the surgery than when it was. The first branchial cleft anomaly does not always exist superficial to the facial nerve. In a total of 83 cases, 47 of the anomalous tracts were identified superficial to the facial nerve, 25 were deep to and 11 were between the branches. Guo et al. in Beijing, China reported 17/41, 17/41 and 7/41 in the same order [4]. Li et al. in Shanghai, also in China reported 21/30, 3/30 and 6/30 [5].
The facial musculature arises from the second branchial arch and spreads into the face through the fused cleft area, accompanied by the facial nerve branches, from sixth to eighth week [6]. The parotid gland arises near the angle of mouth at the sixth week and grows laterally into the pes anserinus area in the seventh to eighth weeks. The relation between the first brachial anomaly and the facial nerve depends on the path of the musculatures [7].
In the cases with an opening to external auricular canal, it is relatively easy to begin the surgery. In the cases without it, the surgeon is ought to find where the anomalous structure is and the relation with the facial nerve. Identifying facial nerve branches is not easy in cases with scar formation. Usage of a nerve monitor is recommended [8].
In our case, repetitive inflammation below the mandibular angle was seen. With the typical symptom, with the existence of cord structure attaching backside of intertragal notch, which was passing into the parotid gland, and with the noticed string structure beneath the induration at the first surgery, we concluded that she had the first branchial cleft anomaly. Though MRI and CT scans could not detect any cyst or fistula, it can be speculated that the first branchial anomaly remained in rudimentary form in our case, mostly so thin a string-like structure that they could not find out. CT scan, taken when she had severe swelling and high fever, clinically obvious with pus accumulation, did not show cystic structure but swollen parotid gland. Contrast between them was not high.
Histologically, no epithelial cells nor lumen was identified inside of it. The epithelial structure was presumed to have been small and escaped from the slices for histology.
CONFLICT OF INTEREST STATEMENT
None declared.



