-
PDF
- Split View
-
Views
-
Cite
Cite
Hemail M Alsubaie, Maisa B Alsmadi, Eidah F Aljuaid, Bilateral peritonsillar abscess: a case study and literature review, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa112, https://doi.org/10.1093/jscr/rjaa112
Close - Share Icon Share
Abstract
While peritonsillar abscesses are the most common deep neck infections, bilateral forms are rare. A peritonsillar abscess occurs when pus accumulates in the peritonsillar space, located between the tonsils and superior constrictor muscle, causing medial displacement of the uvula, trismus, odynophagia or even upper airway obstruction. High clinical suspicion is needed to diagnose bilateral peritonsillar abscess due to frequent history, computerized tomography scan of the neck with IV contrast facilitates accurate diagnose and a full assessment of the patient. Incision and drainage are needed to evacuate the pus along with systemic antibiotics to relieve patient symptoms followed by interval tonsillectomy, which usually done after 6 weeks.
INTRODUCTION
Peritonsillar abscesses are the most common deep neck infections and often occur as a complication from acute tonsillitis. Unilateral peritonsillar abscesses are relatively common, but bilateral presentation is rare [1]. Diagnosis is challenging and requires high clinical suspicion and proper examination to rule out other differential diagnoses. Most researchers agree that both aspiration with a needle and incision and drainage are the optimal clinical approaches to managing peritonsillar abscesses and are equally effective for the management of the disease. Quinsy tonsillectomy is a reliable and safe procedure, advised for bilateral cases, immunocompromised patients, or if no improvement occurs in response to antibiotics or incision-drainage of the abscess [2].

CT scan with IV contrast, axial view showing bilateral peritonsillar abscess with rim enhancement.
CASE PRESENTATION
A 35-year-old female patient from the southern region of Saudi Arabia presented at our institution. She was without medical illnesses with a history of three caesarian sections and acute tonsillitis for 2 weeks. She was treated with oral and intravenous antibiotics for 4 days but did not improve. The patient presented with odynophagia, dysphagia, change of voice, salivary drooling, decreased oral intake and fever for 3 days.
Examination revealed that the patient appeared sick, pale, with a muffled voice known as hot potato voice, mild trismus with limited mouth opening, with no stridor or respiratory distress, bilateral lateral neck lymph node enlargement, fever, enlarged peritonsillar spaces and bilateral tonsils with exudates and uvula pushed anteriorly, posterior pharyngeal wall not visualized and a narrow airway. Her oxygen saturation from room air was over 95%, temperature 37.8°C, heart rate 138 beats/min, WBCs 9.59, C-reactive protein 270 and erythrocyte sedimentation rate 55. A computerized tomography of her neck with intravenous contrast showed bilateral hypodense peripheral enhanced cavities filled with fluids in the peritonsillar spaces, with left multilocular appearance (Fig. 1). Bilateral cervical lymph nodes were noted.
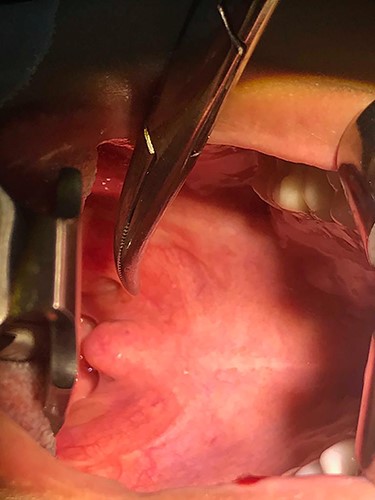
Intraoperatively, the patient was intubated with an endotracheal tube under general anesthesia by video-assisted laryngoscope, about 5 ml was aspirated from each side at the most prominent site, followed by incision at the same site of aspiration. A culture of the aspirated pus showed negative growth with few pus cells. The patient was prescribed intravenous fluids, intravenous analgesics, dual intravenous antibiotics and intravenous steroids during the perioperative period. All symptoms resolved completely within 3 days, and the patient was discharged 3 days after the procedure. The patient underwent a tonsillectomy 6 weeks later without complications (Fig. 2).
DISCUSSION
Bilateral peritonsillar abscesses are rare despite unilateral peritonsillar abscesses being the most common complication of acute tonsillitis [3]. Peritonsillar abscesses affect young adults aged 20–40-years old with a male-to-female ratio of 2:1 [4], which is 1.9–2.4% of reported cases of quinsy tonsillectomies [5]. Peritonsillar abscess is an accumulation of pus inside the peritonsillar space between the superior constrictor muscle and tonsillar capsule [6]. The usual symptoms of a unilateral peritonsillar abscess are sore throat associated with odynophagia, high-grade fever and drooling. It can cause upper airway obstruction with difficult operative intubation due to trismus. Although the most common organism cultured from peritonsillar abscesses is group A beta-hemolytic streptococci (Streptococcus pyogenes), it is usually unnecessary for diagnosis or the treatment plan [4]. A bilateral picture of the abscess gives an idea of other conditions, such as acute follicular tonsillitis, lymphoma, infectious mononucleosis or parotid and submandibular gland mass [5, 6]. Its incidence can be isolated or caused by infectious mononucleosis [7]. Early surgical intervention is highly recommended for fast recovery and resolution of the disease, especially once the abscess is well-formed, and to prevent airway obstruction or spread to other neck spaces such as the parapharyngeal space, mediastinum or base of the skull [1, 8]. Since the 1980s, needle aspiration has been considered the primary treatment choice as it offers diagnostic and therapeutic capabilities and other medical choices are lacking [5]. Other treatment approaches for peritonsillar abscesses include incision and drainage or quinsy tonsillectomy. There is not much difference between managing unilateral and bilateral abscesses, the main aim is to avoid complications that could be worse with bilateral presentation. Both are managed by needle aspiration to relieve symptoms and as a diagnostic test, then by incision and drainage as the optimal treatment of most abscesses in the body including peritonsillar abscess whether unilateral or bilateral. Researchers have found that these options are the most effective with lowest recurrence rates and later less need for a quinsy tonsillectomy, and that incision and drainage or a quinsy tonsillectomy can be considered when needle aspiration confers no improvement [9]. Airway security at emergency presentation is crucial and life-saving [10]. Immunocompromised patients need more attention when presenting with such a disease as they might need a quinsy tonsillectomy as the first treatment line to avoid complications such as deep neck spaces infections and abscess collections. Poor socioeconomic status and poor oral hygiene should be looked for in such patients as they might be risk factors for bacterial contamination leading to the progression of the disease and delayed healing.
In conclusion, bilateral peritonsillar abscess is a rare complication from acute tonsillitis that needs high clinical suspicion as the patient could have an airway obstruction causing potential mortality. It is essential to inform the anesthesiologist about the possibility of difficult intubation due to trismus. Computerized tomography scan of neck with IV contrast is the diagnostic tool best suited to confirm the diagnosis and extension as if abscess look multilocular in computerized tomography that should be kept in mind during procedure. Usually aspiration or incision and drainage are done to exclude other differential diagnoses. Incision and drainage are the optimal management approach preceded by aspiration as with unilateral peritonsillar abscesses. Continuous follow up after discharging patients is beneficial to rule out recollection and improved quality of life. A tonsillectomy 6 weeks after abscess presentation is curative for the patient and decreases disease recurrence.
Conflict of Interest statement
None declared.
Funding
None.



