-
PDF
- Split View
-
Views
-
Cite
Cite
Dominic Brown, Georgios Tsampoukas, Loss of libido in a man with an incidental Leydig cell tumour of the testis: a rare tumour discovered following an isolated common complaint, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa241, https://doi.org/10.1093/jscr/rjaa241
Close - Share Icon Share
Abstract
Leydig cell tumours (LCTs) are rare testicular stromal neoplasms classically presenting with a painless testicular mass or swelling in adults. Symptoms secondary to hypogonadism may occur resulting from the hormonal activity of these tumours. Loss of libido is described in LCTs in conjunction with other symptoms; however, no case has reported this as the sole presenting feature. We describe the case of a 42-year-old man presenting to his General Practitioner with loss of libido and no other features suspicious of testicular cancer. Ultrasound performed due to an unrelated epididymal cyst detected an incidental mass confirmed as a benign LCT following radical orchidectomy. Biochemical markers remained normal throughout and following treatment his libido returned to normal. This case may serve as a reminder for clinicians to maintain a high index of suspicion for testicular neoplasms in patients with features of hypogonadism in the absence of classical features for testicular cancer.
INTRODUCTION
Leydig cell tumours (LCTs) are rare testicular stromal neoplasms derived from the Leydig interstitial cells of the testicle located adjacent to the seminiferous tubules [1]. Despite comprising the most common interstitial neoplasm of the testis [2], LCTs are rare, accounting for ~ 1–3% of all testicular cancers [3], and follow a bimodal distribution with peak incidence between 5–10 and 25–35 years of age [4].
Presenting symptoms of an LCT can vary and are related either to the local effects of the tumour itself or the systemic features secondary to hormone secretion [3]. Age of presentation can also impact how a patient presents; whilst there may be signs of premature virilisation in the pre-pubescent population [2, 4], adult males frequently report a painless palpable testicular mass or swelling [5] or features secondary to hypogonadism resulting from the tumour-related increase in testosterone transformation to oestradiol [4]. This presents as gynaecomastia in up to 10% of patients [5, 6], whilst less often manifesting itself as infertility and rarely erectile dysfunction associated with loss of libido [4]. Despite loss of libido being a recognised complaint in LCTs, it is rare that this is the only sign or symptom reported by the patient on presentation.
We report a case of an incidental benign LCT in a patient whose only reported symptom was loss of libido, which returned following radical orchidectomy.
CASE REPORT
A 42-year-old man with no past medical history presented to his General Practitioner (GP) complaining of loss of libido over the preceding 3 months. He took no regular medication, reported no relevant family history and was otherwise well in himself. On physical examination, the GP noted a small, fluctuant palpable swelling on the left testis and referred the patient for scrotal ultrasound plus urology clinic review.
In clinic, the patient denied any testicular pain or swelling and did not report any lower urinary tract symptoms or haematuria. On examination, he had a normal right testis and a small, smooth, non-tender cyst-like swelling on the superior aspect of the left testis. General examination was unremarkable with no enlarged lymph nodes or evidence of gynaecomastia.
Initial blood tests demonstrated normal levels of the tumour markers lactate dehydrogenase (LDH), alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG) and a testosterone level in the normal range for a male of his age.
Scrotal ultrasound identified a 14 × 12-mm hypoechoic mass towards the upper pole of the left testis (Fig. 1) reported as suspicious for an intratesticular neoplasm. A 2-cm simple cyst of the left epididymis was also reported. The right testis was normal.
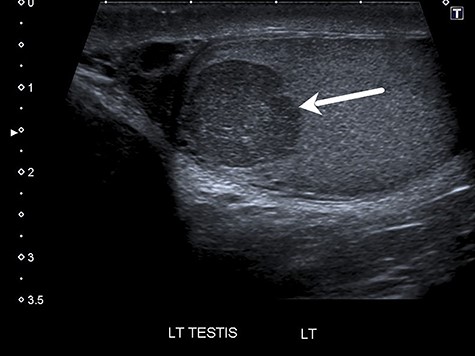
Ultrasound showing 14 × 12-mm hypoechoic mass in the upper pole of the left testis (see arrow).
The case was discussed in a multidisciplinary team meeting and the decision was made to proceed with a radical left inguinal orchidectomy. Subsequent computed tomography scan of the chest, abdomen and pelvis found no evidence of metastases and so no further treatment was considered.
Histology demonstrated a 15 × 10-mm well-defined, tan brown solid nodule with no areas of necrosis or haemorrhage (Fig. 2). The tumour cells stained positive for the immunohistological markers calretinin and MelanA but negative for all other markers (PLAP, BCL-2, CD30, AFP, hCG and cytokeratin). The morphological appearances and immunophenotype were consistent with an LCT and no histological features suggestive of malignancy were present (see discussion).
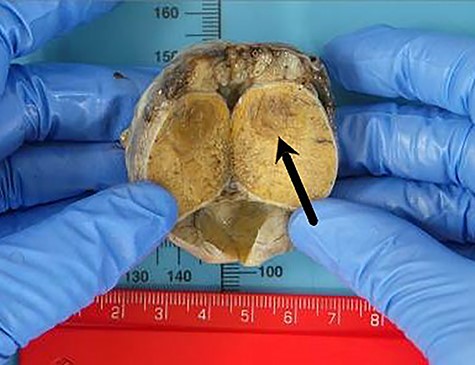
Macroscopic histology of the left testis demonstrating a 15 × 10-mm well-defined nodule in the upper pole (see arrow).
Histology also confirmed the presence of a 25 × 20-mm benign epididymal cyst consistent with that palpated by both the GP and urologist on initial presentation.
The patient underwent repeat blood tests 1-month post-orchidectomy. Testosterone, prolactin, oestradiol and sex hormone-binding globulin all fell within the normal reference range for an adult male and the free androgen index was calculated at 82.3 (normal range ~30–150).
On follow-up, 6-month post-orchidectomy the patient reported he was well with no surgical complications and that his libido had returned to normal.
DISCUSSION
LCTs are rare sex cord–stromal tumours of the testes that generally exhibit a benign course with only 10% of cases in adults demonstrating malignancy [1]. The only reliable criterion for diagnosing a malignant LCT is the presence of proven distant metastases [7]. However, certain histopathological features may suggest malignancy such as large tumour size (>5 cm), vascular invasion, necrosis, infiltrative margins or DNA aneuploidy [5, 8]. None of these features were present on histopathological examination which, coupled with the absence of metastases on imaging, confirms the diagnosis of a benign LCT in this case report.
The presentation of patients diagnosed with LCTs can vary, and although often linked to the tumour’s hormonal activity and secondary hypogonadism, the most common reported feature is testicular swelling or a palpable testicular lump with or without pain [4]. A non-palpable tumour, however, is not uncommon and was found in up to 60% of patients with LCT in one multicentre retrospective study [9]. Loss of libido is a recognised complaint, most often in combination with erectile dysfunction [4], but to date we have found no published report identifying this as the sole presenting symptom.
Serum tumour markers are not typically raised in stromal tumours of the testes, which is consistent with the normal values demonstrated in this case report. According to the European Association for Urology guidelines, AFP, hCG and LDH should be determined prior to orchidectomy for all testicular neoplasms. Whilst at least one of these three markers is raised in up to 59% of patients with germ cell tumours at diagnosis [10], results falling within normal reference ranges cannot be relied upon as ruling out testicular pathology, particularly in the case of stromal neoplasms such as LCTs with expected normal marker values.
This patient presented to the GP with the sole complaint of loss of libido and only underwent subsequent investigation in the form of scrotal ultrasound due to the unrelated presence of a simple epididymal cyst detected following a thorough examination. This case highlights the importance of maintaining a high index of suspicion when considering a diagnosis of testicular neoplasm in patients presenting with symptoms that may be a result of hypogonadism, despite the absence of the classical clinical signs or symptoms such as pain or testicular lump and in the presence of normal biochemical investigations. We hope it will serve as a useful reminder to clinicians when dealing with such presentations.



