-
PDF
- Split View
-
Views
-
Cite
Cite
John Yeh, Pranavan Palamuthusingam, Mucinous cystic neoplasm of the liver: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa220, https://doi.org/10.1093/jscr/rjaa220
Close - Share Icon Share
Abstract
A 50-year-old woman was investigated for epigastric pain. Imaging revealed a multilocular cyst with multiple thin septae within segment IV of the liver, measuring up to 140 mm in diameter. There was associated bile duct dilatation. Given the patient’s symptoms, the size of the cyst and malignant potential, a hemi-hepatectomy was performed. Histopathology demonstrated a cyst lined by columnar mucinous epithelium with underlying ovarian-type stroma. Therefore, the diagnosis was mucinous cystic neoplasm of the liver (MCN-L). MCN-L is a rare disease, and the presence of bile duct dilatation is an even rarer finding. This article presents a case report and review of literature of this entity.
INTRODUCTION
Mucinous cystic neoplasm of the liver (MCN-L) has gathered increasing interest over recent years. Previously called biliary cystadenoma or biliary cystadenocarcinoma, the 2010 World Health Organization (WHO) classification has defined MCN-L as a cyst-forming epithelial neoplasm with ovarian-like stroma and without biliary communication [1]. However, with few cases of MCN-L among the published literature, our understanding of its characteristics is still evolving. We present a case of MCN-L that was managed with hemi-hepatectomy.
CASE REPORT
A 50-year-old woman was referred to our institution with a large complex left liver lobe cyst. She had 3 months of epigastric and right hypochondrial pain, associated with nausea and anorexia. Ultrasound had revealed a large, well-defined septated cystic mass in the left lobe measuring up to a maximum diameter of 140 mm (Fig. 1a). Her laboratory data at the time showed deranged liver function tests, with alkaline phosphatase of 472 IU/L, gamma-glutamyl transpeptidase of 1147 IU/L, alanine aminotransferase of 121 IU/L and aspartate aminotransferase of 86 IU/L. The bilirubin was normal at 7 μmol/L, and she had negative hepatitis and hydatid serology.
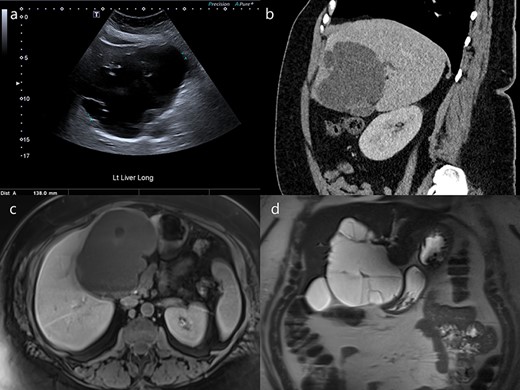
Ultrasound, CT and MRI imaging of the cyst. (a) Ultrasound detected a septated cyst measuring up to 140 mm in diameter. (b) Intrahepatic bile duct dilatation was demonstrated on CT (sagittal). The cyst was (c) hypointense on T1-weighted images (axial) and (d) hyperintense on T2-weighted images (coronal).
Subsequent abdominal computed tomography (CT) demonstrated the large exophytic multi-septated cyst predominantly within segment IV. It had lobulated margins and thin intrinsic septations with subtle post-contrast enhancement, but no enhancing mural nodule or intrinsic calcification. Additionally, there was mild dilatation of the left liver lobe bile ducts, and displacement of the left and right portal veins due to mass effect (Fig. 1b). Magnetic resonance imaging (MRI) of the liver with cholangiopancreatography confirmed an intrahepatic biliary dilatation more pronounced on the left. The cyst contents were homogenously T1 hypointense and T2 hyperintense (Fig. 1c and d).
Overall, a simple cyst was thought unlikely and a provisional diagnosis of biliary cystadenoma or cystadenocarcinoma was made. Given the patient’s age and symptomology, the size of the cyst, biliary compression and risk of malignant transformation, the decision was made for surgical resection rather than observation.
A left hemi-hepatectomy with cholecystectomy was performed. Within the left lobe of the liver was a thin-walled cavity containing brown serous liquid, with multiple loculations and trabeculations. There were two focally roughened, hemorrhagic areas within the cyst (Fig. 2a). Microscopically, this multilocular cyst was lined by a single layer of columnar mucinous epithelium with underlying ovarian-like hypercellular stroma (Fig. 2b and c). The cyst epithelium showed squamous metaplasia without cytological atypia or malignancy and was positive for cytokeratin (CK)7 (Fig. 2d). Therefore, a diagnosis was made of mucinous cystic neoplasm of the liver, without evidence of dysplasia or malignancy.
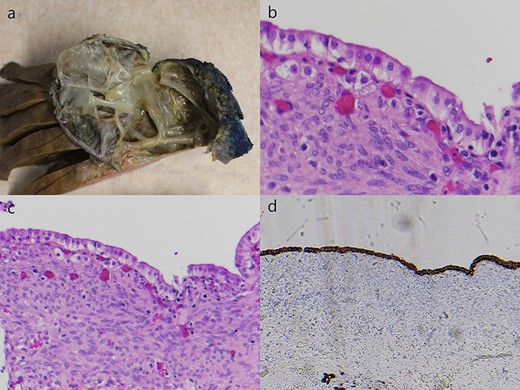
Macroscopic and microscopic features of the cyst. (a) There was a trabeculated and loculated cavity within the left lobe. (b) The cyst was lined by a single layer of columnar mucinous epithelium without cytological atypia (H&E staining, ×200). (c) This epithelium was underlined by an ovarian-like hypercellular stroma (H&E staining, ×100), and (d) was positive for cytokeratin 7 (CK7 staining, ×40).
The post-operative course was uncomplicated, and the patient was discharged on Day 7. She was recovering well by the time of initial follow-up at 4 weeks, with further review planned at 6 months.
DISCUSSION
Our presented case supports much of the current literature on MCN-L. MCN-L is known to be a disease seen almost exclusively in women [1]. Ages have been reported from as young as 21 years to as old as 80 years, with a mean age of around 45 years [1, 2]. While the clinical manifestations are variable, the most common symptom at time of presentation is abdominal pain [1].
Pre-operative diagnosis of MCN-L has been aided by the ready availability of various imaging modalities. Ultrasound is often the first-line modality to detect complex liver cysts; however, it is unable to reliably differentiate between non-neoplastic and neoplastic cysts [3]. Findings on CT and MRI are that of large, solitary and multilocular cystic lesions, with well-circumscribed margins and internal septa [4]. These typically show no communication with the bile duct and do not cause biliary dilatation [5, 6]. Up to 75% occur in the left lobe of the liver, though the reason for this is unclear [2, 7]. While features such as hemorrhagic internal fluid, a solid mural nodule and coarse calcification along the cyst wall or septa are suggestive of malignancy, the identification of MCN-L with associated carcinoma based on imaging alone remains challenging due to the considerable overlap in characteristics [4]. Therefore, complete surgical resection is required, and it is suggested that a large (>100 mm) cyst at initial presentation, increasing size on surveillance and symptomatic cysts are indications for resection [2].
Definitive diagnosis of MCN-L relies on the histological findings. The WHO classification defines MCN-L as a cyst-forming epithelial neoplasm comprising cuboidal to columnar, variably mucin-producing epithelium. Importantly, the presence of an ovarian-type subepithelial stroma is required for diagnosis, and the cyst usually does not communicate with the bile ducts [1]. Additionally, a biliary immunophenotype with expression of CK7 alone is characteristic of benign MCN-L, while expression of gastrointestinal markers CK20, mucin core protein (MUC)1, MUC2, MUC5AC and MUC6 is suggestive of borderline or malignant cases [2].
Regardless of the presence of carcinoma, the prognosis of MCN-L appears to be excellent with complete resection. Around 90% of cases are histologically benign [7, 8]. Local recurrence of benign MCN-L has been reported from 5 months up to 8 years after initial resection, though none of the subsequently resected tumors demonstrated malignant transformation [7]. Overall, no patients with MCN-L, with or without invasive carcinoma, have died from the disease [8].
Interestingly, one aspect that differed between our case and the accepted characteristics of MCN-L was the presence of intrahepatic biliary dilatation. Bile duct dilatation and biliary communication are features classically associated with intraductal papillary mucinous neoplasm of the bile duct and have been used to help differentiate it from MCN-L [5, 6]. Although uncommon, this finding has been seen in other cases of MCN-L. Kunovsky et al. [9] reported a case of a 33-year-old woman with MCN-L and a dilated left hepatic duct on pre-operative imaging, while Rodriguez et al. [10] reported a case of a 35-year-old woman with intrahepatic biliary dilatation requiring pre-operative endoscopic insertion of a right hepatic stent. Two further cases of MCN-L have been reported to show cystic communication with the bile ducts, diagnosed by the post-operative injection of contrast into the bile duct [8]. While intraductal papillary mucinous neoplasm of the bile duct has a high probability of malignancy, no increased risk has been observed with MCN-L even in cases of bile duct involvement [8, 9].
Overall, MCN-L is a rare disease, and further investigation is necessary to better define its characteristics.
ACKNOWLEDGEMENTS
We acknowledge Myo Thu and Shelley Verma for their assistance with the pathology images.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.



