-
PDF
- Split View
-
Views
-
Cite
Cite
Alex Paul Guachilema Ribadeneira, Naysi Cristina Zambrano Martinez, Silvana Alexandra Valencia Valverde, Raúl Ernesto Villacis Peñaherrera, Fabian Medardo Romero Chacón, Andrea Daniela Basantes, Spontaneous jejunoileal perforation as a manifestation of celiac disease—a rare entity: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa219, https://doi.org/10.1093/jscr/rjaa219
Close - Share Icon Share
Abstract
Celiac disease or gluten-sensitive enteropathy is characterized by an autoimmune response in the small intestine triggered by the ingestion of gluten in the diet. It has a prevalence of 0.62% worldwide with considerable variation in incidence among countries. The clinical manifestations of celiac disease differ according to type: the classical type presents with intestinal symptoms, the non-classical type with intestinal or extraintestinal symptoms and the silent type is asymptomatic. Human leukocyte antigens (HLA)-DQ2 (DQA1_05/DQB1_02) are expressed in >90% of patients with celiac disease, and the presence of HLA-DQ2 or HLA-DQ8 (DQA1_ 0301/DQB1_0302) is necessary for its development. One complication of this disease is ulcerative jejunoileitis, a rare condition characterized by chronic idiopathic ulceration affecting the small intestine that can cause intestinal perforation resulting in high morbidity.
INTRODUCTION
Celiac disease is defined as a multisystemic disorder that is triggered by the ingestion of gluten. The disease has high morbidity and mortality in symptomatic cases. However, in the majority of cases, the disease remains undetected, which leads to the development of complications that increase morbidity and mortality. Patients with undiagnosed celiac disease may have atypical or mild symptoms that remain undetected for a prolonged period and possibly throughout life. Ulceration with free perforation is a rare occurrence in patients with celiac disease, and the most common location is the jejunum.
Here, we present a case of ulcerative jejunoileitis with perforation as a complication of celiac disease. Because this is an uncommon pathology and there are no published cases in our region, it needs to be considered in all patients that present with spontaneous small bowel perforation and acute abdomen.
CASE REPORT
A 64-year-old woman presented with a history of untreated thyroid cancer and chronic diarrhea for 7 months without a diagnosis. The patient presented to the emergency department with sudden abdominal pain of moderate intensity and of a colicky quality, localized to the mesogastrium and irradiating to the hypogastrium, accompanied by several episodes of vomiting. Physical examination showed a distended abdomen that was painful on palpation at the hypogastrium and vague peritoneal symptoms. Additional tests showed neutrophilic leukocytosis and moderate hypokalemia. A computed tomography scan of the abdomen and pelvis with and without contrast revealed multiple mesenteric lymph nodes in addition to ileal intestinal enhancement with a small amount of free liquid in the abdominal cavity, a hydropic gallbladder and a distended appendix. A diagnostic laparoscopy was performed and later converted into an exploratory laparotomy because of the presence of free intestinal liquid in the cavity caused by small bowel perforation (Fig. 1A).
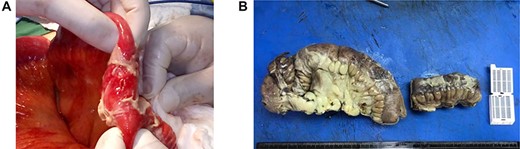
(A) Fibrinopurulent exudate and terminal ileal perforation at 20 cm from the ileocecal valve, measuring 0.3 cm in diameter. Pre-perforated areas are located at 40 and 60 cm from the ileocecal valve. (B) Resection of the ileum.
Ileal resection (Fig. 1B) with ostomy and abdominal lavage were performed, and a negative pressure drainage system was placed. The surgical procedure was performed without complications, and the patient was transported to the recovery room to begin antibiotic therapy.
In the immediate postsurgical period, increased ileostomy production of >2000 ml in 24 hours was observed, and the patient was therefore started on loperamide treatment. Immunological tests were performed considering a differential diagnosis of celiac disease, and the results were as follows: positive transglutaminase IgA antibodies, positive IgG and negative anti-endomysial antibody.
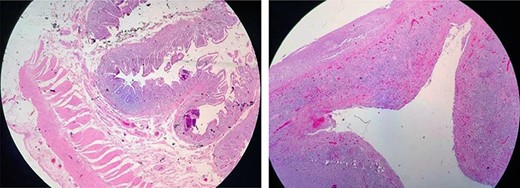
The surgical histopathology report was negative for malignancy and showed reactive changes with decreased villi crypts; a severe mixed inf lammatory infiltrate of the lamina propria was predominantly lymphoplasmacytic with accumulation o eosinophils and histiocytes,whichwere indicative of acute ulcerative ileitis with perforation. No microorganisms were identified (Fig. 2). Intestinal traffic was restored at 10 weeks. A side-to-side jejunocecal anastomosis was performed. The patient showed good evolution with a gluten-free diet and an improved clinical outcome. The patient was discharged from the surgical ward and scheduled for follow-up at the Department of Gastroenterology.
DISCUSSION
The prevalence of celiac disease is low at 0.62%, and it is more frequent among women than men [2]. It is most commonly diagnosed in adults between the fifth and sixth decades of life. It is characterized by an autoimmune reaction against the small bowel triggered by gluten in the diet. Ulcerative jejunoileitis is a complication of celiac disease that is characterized by the presence of chronic idiopathic ulceration affecting the small intestine [3]. Ulceration is mostly localized to the jejunum and occasionally the ileum, whereas localization to the colon is rare [2].
The clinical presentation includes symptoms of malabsorption, diarrhea and steatorrhea, as well as other symptoms such as fever, abdominal pain and weight loss. The results of analyses often show hypoalbuminemia associated with protein-losing enteropathy, iron- and folate-deficiency anemia and hydroelectrolytic disturbances. The pathologies that cause spontaneous perforation of the small intestine include intestinal lymphoma, Crohn’s disease and infection, which need to be considered in the differential diagnosis [4].
The complications include digestive hemorrhage, intestinal perforation and intestinal obstruction; the latter two constitute indications for emergency surgery [4, 5] and are associated with higher mortality [6]. Regarding its diagnosis, abdominal computed tomography scan typically shows mesenteric adenopathy and splenic atrophy. A definitive diagnosis is frequently made based on laparotomy with resection of the affected segments. Anti-transglutaminase and anti-endomysial antibodies, and HLA-DQ8 positivity are common findings.
The treatment of patients with celiac disease is complex because there are currently no known treatments capable of modifying the course of the disease. One possibility is corticosteroid treatment; however, the patients rarely respond to this treatment, and steroids are associated with an increased risk of perforation. Surgical resection of the affected segments can have a curative effect in some patients in addition to ruling out the presence of lymphoma, although most patients remain symptomatic after surgery as in the present case [5]. Celiac disease associated with lymphoma has a poor prognosis, and one-third of patients die despite strict adherence to a gluten-free diet.



