-
PDF
- Split View
-
Views
-
Cite
Cite
Saifullah Mohamed, Akshay J Patel, Yassir Iqbal, Khurum Mazhar, Uday Dandekar, Sunil Bhudia, Type B aortic dissection repair using a Thoraflex hybrid prosthesis in a setting of aberrant left vertebral artery, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa218, https://doi.org/10.1093/jscr/rjaa218
Close - Share Icon Share
Abstract
Type B aortic dissection (TBAD) is often managed conservatively with intervention reserved for complicated cases. Strategies for complicated and uncomplicated TBAD can involve optimal medical therapy, thoracic endovascular aortic replacement and open surgical repair of TBAD with replacement of the affected segment of aorta and reimplantation of aortic branches. The frozen elephant trunk technique has been reported to be a successful surgical strategy in patients with complicated TBAD, particularly in patients who possess unfavourable aortic arch anatomy for endovascular stenting or at increased risk of retrograde Type A aortic dissection. The Thoraflex is a commercially available aortic graft, manufactured by Vascutek®. We describe a successful case of addressing complicated TBAD with rare variant aortic anatomy using a Thoraflex hybrid frozen elephant trunk graft and reimplantation of the aberrant left vertebral artery to the perfusion limb of the Thoraflex graft.
INTRODUCTION
Type B aortic dissection (TBAD) is often managed conservatively with intervention reserved for complicated TBAD [1]. Aortic dissection is incorporated into the spectrum of acute aortic syndrome that also includes intramural haematoma and penetrating aortic ulcer. Furthermore, TBAD has a different management strategy and urgency to Type A aortic dissection (TAAD), involving the ascending aorta [1]. Strategies for complicated and uncomplicated TBAD can involve optimal medical therapy, thoracic endovascular aortic replacement (TEVAR) and open surgical repair of TBAD with replacement of the affected segment of aorta and reimplantation of epiaortic branches [1]. Various surgical approaches and strategies can be utilized to replace the affected aorta and restore true luminal patency and obliteration of the false lumen, inherently dependent on the pathology [2]. The fate of the false lumen and ensuing management has been demonstrated to be of prognostic importance [3]. Surgery for acute TBAD is associated with a high 30-day mortality especially for surgery involving the aortic arch and thoracoabdominal aorta, comparatively the 30-day mortality for chronic TBAD is considerably smaller [4]. The frozen elephant trunk (FET) technique has been reported to be a successful surgical strategy in patients with complicated TBAD, particularly in patients who possess unfavourable aortic arch anatomy for endovascular stenting or at increased risk of retrograde TAAD [5]. The Thoraflex is a commercially available aortic graft, manufactured by Vascutek®, which is comprised of a four-branch Gelweave graft, a distal endograft with an incorporated sewing collar proximal to the endograft [6]. We describe a successful case of addressing complicated TBAD with rare variant aortic anatomy using a Thoraflex hybrid FET graft and reimplantation of the aberrant left vertebral artery to the perfusion limb of the Thoraflex graft.
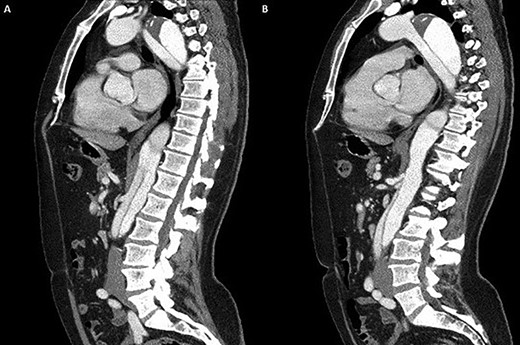
(A) Coronal section demonstrating the distal arch with the left vertebral and subclavian arteries visible; (B) coronal section demonstrating aneurysmal enlargement of the descending thoracic aorta and Type B dissection.
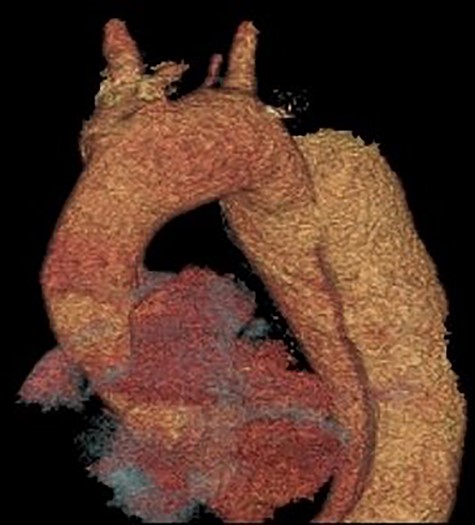
3D reconstruction of the CT scan demonstrating the four-vessel arch configuration with the aberrant left vertebral artery located in the Zone 2 region.
CASE DISCUSSION
A 52-year-old gentleman presented to our institution with a previous history of TBAD (diagnosed 3 years previously), which was managed conservatively. His comorbidities included hypertension and excision of a left frontal cavernoma with no family history of aortic aneurysm or dissection. Following his initial presentation of chest pain, the patient had remained asymptomatic and stable. Surveillance management was initially instituted and the case discussed at the aortic multidisciplinary meeting. Due to retrograde extension of the TBAD into the distal arch, persistence of the false lumen, increasing descending aortic dimensions (6.0 cm) and an anomalous left vertebral artery originating from the aortic arch, the patient proceeded to aortic arch surgery and antegrade deployment of the stent into the descending aorta with a FET graft (Figs 1, 2). Preoperative coronary angiography and transoesophageal echocardiography revealed no coronary artery disease and a competent trileaflet aortic valve with preserved left ventricular function.
Cardiopulmonary bypass support was established using right atrial drainage and right axillary artery return. During cooling to 18°C, the aorta and epiaortic arch vessels were mobilized and encircled with tapes. At 21°C, the heart was fibrillated, aortic cross-clamp applied and antegrade cold blood intermittent cardioplegia administered to arrest the heart. At 18°C, neuroprotective protocol (topical ice to the head, intravenous steroids and mannitol administration with near infrared spectroscopy monitoring of cerebral saturations) was instituted and circulatory arrest commenced. The ascending aorta was transected 1 cm proximal to innominate artery and aortic arch inspected. Selective antegade cerebral perfusion was commenced. The aortic arch was divided in Zone 2 in order to protect the recurrent laryngeal nerve. The origin of the aberrant left vertebral artery and left subclavian artery were oversewn with a running 4/0 prolene suture. A 30/32/150 mm Thoraflex stent graft was deployed into the true lumen of the descending aorta. The cuff on the stent graft was anastomosed to the distal arch. Attention was then directed to the left common carotid and innominate arteries that were fashioned and anastomosed to the corresponding grafts on the stent graft. The aortic cross clamp was applied on the ascending aorta portion of the stent graft and total body circulation and rewarming was reinstituted. The ascending aorta was anastomosed to the stent graft 1 cm proximal to the innominate artery. A thorough de-airing drill was undertaken, the aortic cross clamp released and heart perfused. The graft on stent graft corresponding to the left subclavian artery was anastomosed and the origin on the aortic arch was oversewn. A 6-mm Dacron graft was then anastomosed to the transected left vertebral artery and origin on the aortic arch oversewn. The 6-mm Dacron graft was then anastomosed to the 8-mm side arm on stent graft corresponding to the perfusion arm. When fully rewarmed, cardiopulmonary bypass support was successfully weaned off and patient was in sinus rhythm requiring no inotropic support. Postoperatively, the patient made an uneventful recovery and was subsequently discharged home without complications and seen in the outpatient clinic as part of their routine surveillance. Computed tomography (CT) imaging performed as an outpatient demonstrated normal graft appearances, aortic arch and epiaortic vessel configurations (Fig. 3).
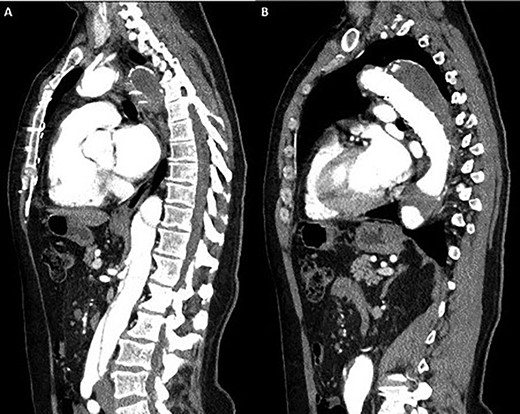
Coronal section CT scan images demonstrating the newly arranged epiaortic reconfiguration on left (A) and on the right (B) the deployed FET and antegrade flow in the descending thoracic aorta through the true lumen.
DISCUSSION
Our case demonstrates the successful use of FET for complicated TBAD as demonstrated previously [10]. The aberrant left vertebral artery originating directly from the aortic arch in the Zone 2 region is the most commonly observed variant, its incidence in a four-vessel epiaortic vessel configuration ranges from 0.68 to 5% [7]. Furthermore, an aberrant left vertebral artery is associated with a higher incidence of arterial dissection ranging from 0.9 to 1.9% [8]. Concerning aortic arch anomalies, the anatomical configuration of an aberrant left vertebral artery in the Zone 2 region pertains to challenging anatomy for TEVAR deployment. However, hybrid TEVAR with stent deployment into the conventional Zone 2 position and cervical transposition of the left vertebral artery to the left common carotid artery has been described [9]. Similarly, hybrid TEVAR with supra-aortic total debranching of the epiaortic vessels and cervical transposition of the left vertebral artery to the left common carotid artery with stent deployment into the Zone 2 position has also been reported [10]. Although not previously described, the surgical technique of reanastomosing the aberrant left vertebral artery to a Dacron graft and subsequent anastomosis to the perfusion limb of the Thoraflex graft mitigates the need for any concomitant cervical anastomosis of the aberrant left vertebral artery and favourably addresses this rare anatomical variation.
ACKNOWLEDGEMENTS
FINANCIAL SUPPORT
None to declare.
CONFLICTS OF INTEREST STATEMENT
None to declare.



