-
PDF
- Split View
-
Views
-
Cite
Cite
Ahmed Alhumidi, Abdulmalik Alqahtani, Metastatic pleural mesothelioma presenting initially as multiple gastric and colonic polyps, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa203, https://doi.org/10.1093/jscr/rjaa203
Close - Share Icon Share
Abstract
It is extremely rare for malignant mesothelioma to present as gastrointestinal polyps. This case report documents the presentation of malignant mesothelioma in a 72-year-old as rectal bleeding and weight loss. Endoscopically, there were multiple gastric and colonic polyps. Histopathologically, there were atypical cells in the lamina propria with benign surface epithelium. The cells tested positive for cytokeratin, calretinin and D2–40 and negative for CD45, CD117, Ber-EP4 and CEA, confirming the diagnosis of metastatic mesothelioma. A computed tomography scan of the chest showed nodular thickening of the left lower pleura that was compatible with a diagnosis of primary pleural mesothelioma. We conclude that metastatic mesothelioma can sometimes present as gastrointestinal polyps.
INTRODUCTION
Mesothelioma is a tumor originating from mesothelial cells lining the serosal cavities. It usually presents between the fifth and seventh decade of life and can be difficult to diagnose because of the vagueness of the presenting symptoms. Because they are most often rapidly fatal, distant metastases are rarely detected at presentation. In this study, we describe an extremely rare case of pleural mesothelioma that presented initially as multiple gastric and colonic polyps.
CASE REPORT
A 72-year-old, non-smoking male with no previous medical or surgical history presented with a 3-month history of rectal bleeding and weight loss. There was no family history of colorectal cancer or familial polyposis. All physical examination findings were normal except for a mild paleness. His blood profile was normal except for mild microcytic hypochromic anemia. Urine and stool analyses were also normal. An ultrasound of his abdomen revealed no abnormalities. An esophagogastroduodenoscopy revealed nothing abnormal in the vocal cords, esophagus, gastroesophageal junction or duodenum, but there were three sessile polyps identified in the gastric body. A colonoscopy then revealed colonic sessile polyps, some of which were ulcerated. The gastric polyps and some of the colonic polyps were ablated and sent for pathological examination.
The polyps were received in formalin and measured between 0.4 and 0.6 cm. A paraffin-embedded tissue was sectioned at 3 microns and multiple levels were evaluated with routine hematoxylin and eosin stain. Microscopic examination revealed that most of the surface of this polyp was covered by normal but focally eroded gastric and colonic mucosa. The lamina propria was infiltrated by tumor cells that were arranged in solid nests with focus of glandular structures lined by single layer of cuboidal cells (Fig. 1). The tumor cells had rounded nuclei with fine chromatin and visible nucleoli. The cytoplasm was abundant and eosinophilic.
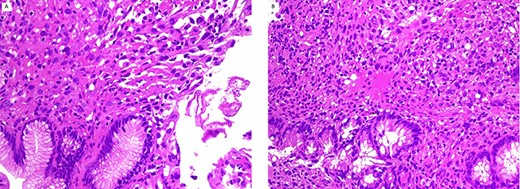
gastric (A) and colonic (B) polyps show neoplastic cells in lamina propria with normal mucosa (H/E stain ×200).
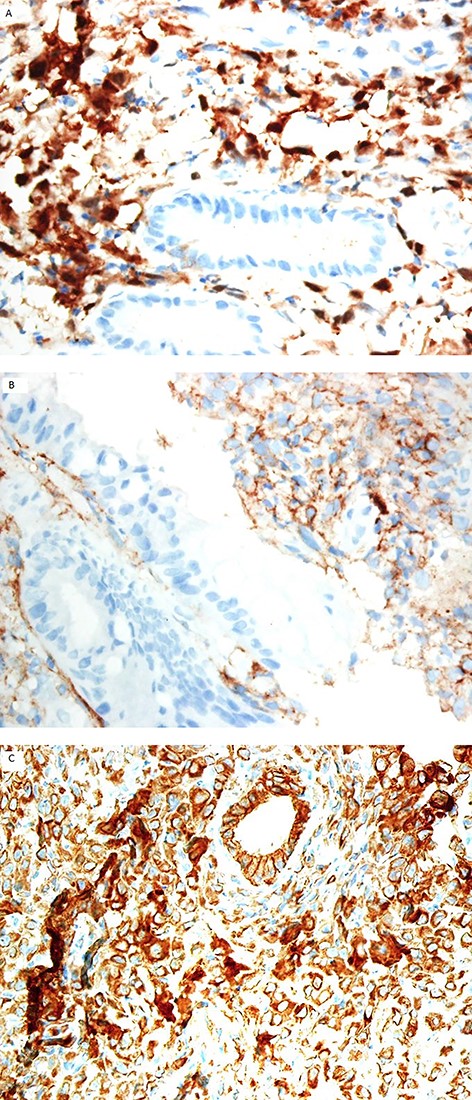
The neoplastic cells are positive for calretinin (A), and D2–40 (B) immunostain. Cytokeratin is positive in the neoplastic cells and background non-neoplastic mucosa (C); (immunohistochemistry stain ×200).
Mucicarmine stain was negative in the tumor cells. Immunohistochemical studies (Fig. 2) showed positive staining for cytokeratin, calretinin and D2–40; and negative for carcinoembryonic antigen (CEA), CD45 and CD117, Ber-EP4, cytokeratin 7 and cytokeratin 20. A diagnosis of metastatic mesothelioma was made.
The patient underwent computed tomography (CT) of the chest and abdomen. The CT scan showed nodular thickening of the left lower pleura (Fig. 3). The patient did not return for the scheduled follow-up appointments.
DISCUSSION
Malignant mesothelioma is a rare neoplasm derived from the mesoderm of the pleura or peritoneum. Most patients die from respiratory distress because of tumor growth. To date, distant metastasis from mesothelioma was considered unusual, with expansion of the local tumor being considered the most frequent cause of death. However, more and more cases of hematogenous metastasis are been recognized at autopsy. The metastatic sites are the liver, adrenal gland, kidney and bone [1, 2].
There are three primary histologic types of mesothelioma: [1] epithelioid; [2] sarcomatoid; and [3] mixed. Epithelioid tumors consist of small or large epithelium-like cells, often demonstrating secretory vacuoles, arranged in acinar or papillary structures. The sarcomatoid type typically consists of spindle-shaped cells and bundles of collagenous fibers arranged in sheets. Mixed tumors show a combination of these two histologic types [3, 4]. Useful immunohistochemical markers confirming mesothelial origin and excluding the more common adenocarcinoma are positive markers for calretinin, D2–40 and WT1 and negative markers for CEA, B72.3 and B72.3 [5, 6].
There have been 15 reported cases of mesothelioma presenting as gastrointestinal metastasis. The gastrointestinal sites of metastatic disease were reported as follows: one pancreatic, three gastric, four duodenal, two in the small intestine, two in the colon, two with metastasis in both the small and large bowels and one rectal metastasis. Malignant mesothelioma presenting initially as gastrointestinal polyps is extremely rare, with only one reported case of an initial presentation of a rectal polyp [7]. The histopathological diagnosis is challenging, because it can easily be misidentified as adenocarcinoma. In our case, immunohistochemical staining was an important tool in differentiating between the two, as positive results for calretinin and D2–40 and negative results for CEA were helpful in distinguishing mesothelioma from adenocarcinoma.

CT scan of the chest reveals nodular thickening (arrow) of left pleura.
We conclude that metastatic disease is uncommon at the time of initial diagnosis of malignant mesothelioma. This report documents an extremely rare case of pleural mesothelioma that presented initially as multiple gastric and colonic polyps. Microscopic diagnosis is difficult and a full clinical history, radiological correlation and immunohistochemical studies are needed for a successful diagnosis.
ACKNOWLEDGMENTS
The authors extend their thanks to the Deanship of Scientific Research at King Saud University for funding this work.
CONFLICT OF INTEREST
The authors declare no conflicts of interest regarding the publication of this paper.



