-
PDF
- Split View
-
Views
-
Cite
Cite
Emanuele Gatta, Sara Schiavon, Gabriele Pagliariccio, Perla Persechini, Luciano Carbonari, Pararenal aortic aneurysm in situs inversus totalis: open repair with right retroperitoneal approach, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa197, https://doi.org/10.1093/jscr/rjaa197
Close - Share Icon Share
Abstract
Situs inversus totalis (SIT) refers to a mirror-image reversal of the internal organ position. The coexistence of abdominal aortic aneurysm and SIT is extremely rare; very short series have been reported; therefore its prevalence has never been estimated. The presence of anatomical anomalies could increase operative risk. The authors describe a case of successfully repaired pararenal abdominal aortic aneurysm with a right retroperitoneal approach in situs inversus totalis.
INTRODUCTION
Situs inversus totalis (SIT) is a rare autosomal recessive disorder which is characterized by a mirror-image reverse position of thoracoabdominal viscera with an estimated prevalence of live births 1/10.000 [1].
The transposition of the organs may be associated with other congenital anomalies, such as pancreatic fibrosis, renal dysplasia, biliary atresia and congenital heart disease [2].
The presence of aortic aneurysm in SIT is really uncommon, and the management could be controversial. Cardiovascular, gastrointestinal and urinary systems anomalies could increase operative risk.
In literature there are few series reporting aortic aneurysm associated with SIT. Good results are reported with median laparotomic approach (in elective and emergency setting) and in endovascular treatment [3–6].
To our knowledge this is the first case in the literature about a successful elective open repair of a pararenal aneurysm with right retroperitoneal approach, in a patient with SIT.

Operative room view showing mirrored setup as compared to routine thoraco–phreno–laparotomy access.
REPORT
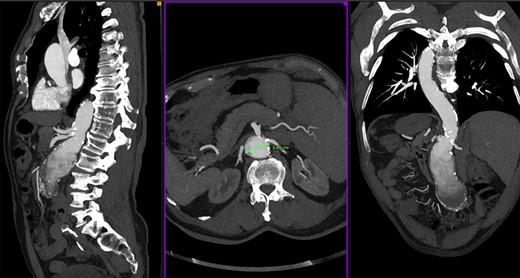
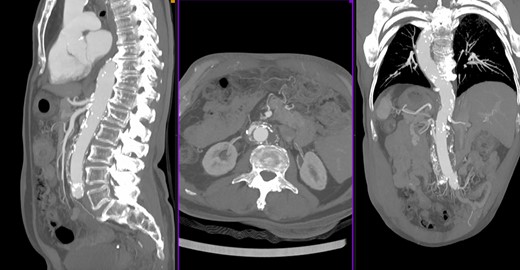
We report a case of a 73-year-old man with known SIT and past medical history of hypertension and dyslipidemia, no other comorbidities (ASA referred to our center for a specific abdominal pain); an US exam was performed, and an abdominal aortic aneurysm (AAA) was found. A followed computed tomography scan showed a 6 × 7 cm pararenal aortic aneurysm (pAAA). The pAAA was extended caudally to the aortic bifurcation with no evidence of rupture (Fig. 1). The diameter of the aorta at lower left renal artery was of 36 mm. The origins of the others visceral vessels were very close and in a short aortic segment. As we usually make for complex aortic cases, a careful multidisciplinary evaluation of comorbidities was performed. Therefore we have proposed an open repair with supraceliac clamping and visceral protection with left–left (anatomically right) heart bypass (LHB). Operation room setup, patient–surgeon position and pump placement were mirrored as compared to routine thoraco–phreno–laparotomy access (Fig. 2). Under general anesthesia, both surgical right axillar and femoral arteries were prepared. We used the axillar artery for the LHB in-line. The femoral artery was prepared for the line-out of the shunt in eventual need of total thoracoabdominal replacement with a long-time perfusion. By a right retroperitoneal approach, we prepared the aorta up to below the diaphragm. Pillars of the diaphragm were sectioned to prepare the better site to clamp the aorta. After systemic heparinization, the aorta was clamped above the celiac trunk. The aorta was opened; both renal arteries, superior mesenteric artery and celiac trunk were cannulated with 9-Fr Pruitt catheters connected to the pump. Therefore, the visceral vessels and the renal arteries were perfused with isothermic blood from the LHB circuit (Medtronic Biomedicus 560 centrifugal pump). Both common iliac arteries were endo-clamped with Fogarty catheters. The left renal artery was disconnected, and an oblique end-to-end anastomosis between the proximal aorta (including the visceral vessels and the right renal artery takeoffs) and a straight 18-mm Dacron graft was performed. The distal anastomosis was constructed at the level of the aortic bifurcation, and subsequently the left renal artery was replaced on the tube graft with T-L anastomosis (Fig 3). Postoperative course was uneventful, and the patient was discharged on 6th postoperative day. Follow-up CT scan 6 months after the intervention showed a good treatment of the aneurysm with a patency of all visceral vessels (Fig. 4).

Intraoperative view showing left renal artery replacement on the tube graft with T-L anastomosis, renal perfusion guaranteed by Anatomically right heart bypass.
Informed consent has been verbally obtained from the patient for publication of the case report and accompanying images.
DISCUSSION
As mentioned in the recent European Society for Vascular Surgery AAA Guidelines, there is no general agreement on how to define aneurysms with short necks and/or involving the visceral arteries. Juxtarenal or pararenal AAA (JRAAA) is defined as an aneurysm extending up to but not involving the renal arteries, necessitating suprarenal aortic clamping for open repair. Suprarenal AAA (sRAAA) is defined as an aneurysm that extends up to the superior mesenteric artery, involving one or both renal arteries to be repaired. The distinction between a SRAAA and a Crawford type IV thoracoabdominal aortic aneurysm (TAAA) is not clearly defined [7].
In the case treated, there is an involvement of the left renal arteries with a very close origin of the superior mesenteric artery and celiac trunk. According to this anatomic issue, we planned a retroperitoneal approach to a safer proximal clamping and anastomosis. Furthermore the closeness of the visceral vessels origins could have required a complex reconstruction of the aorta as in thoracoabdominal aneurysm. Therefore, we prepared the left–left shunt (anatomically right) to be ready for a complete visceral perfusion. We used the right axillar artery for the line-in of the shunt otherwise thoracic aorta of inferior pulmonary vein to reduce the invasiveness avoiding the thoracotomy.
Open TAAA-pararenal AAA repair is a high-demanding intervention being associated with considerably mortality and morbidity. In this setting custom-made fenestrated (FEVAR) and branched (BEVAR) endovascular repair has emerged as a valid alternative option. However, these procedures are not fit for all anatomical settings.
In the present case, the endovascular treatment was excluded due to the closeness of the target vessels that could be unfavorable to a safety customized endograft placement. Furthermore, by an accurate preoperative evaluation, no contraindications to the open surgery were highlighted.
In conclusion, literature describes a limited number of cases of aortic aneurysm in SIT treated by open repair technique. We chose the right posterior approach to control the aorta above visceral arteries. This choice represented a challenge but also a safer surgery.
Despite the limited number of cases described, we can conclude that the SIT is not a problem to the open repair with retroperitoneal approach of the pararenal aortic aneurysm.
ACKNOWLEDGMENTS
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.



