-
PDF
- Split View
-
Views
-
Cite
Cite
Sabrina Brar, Carolina Watters, A real ball ache: a case report of acute pancreatitis with an unusual sequelae of events, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa199, https://doi.org/10.1093/jscr/rjaa199
Close - Share Icon Share
Abstract
Acute pancreatitis may present with a myriad of clinical and radiological manifestations. Assessment of the severity and prognosis of the disease is often based on clinical features, laboratory analysis and computer tomography (CT) scans; however, the predictive value of CT is not 100% accurate. We report herein a case with an especially rare sequence of clinical events, manifesting as a septic fluid collection within the inguinal canal that was misdiagnosed as an inguinal hernia on CT imaging. The patient underwent surgical drainage and an orchidectomy to treat the infection. This case illustrates the complexity and severity of acute pancreatitis as well as the challenges in interpreting and relying on diagnostic radiological data.
INTRODUCTION
A diagnosis of acute pancreatitis is confirmed by analysis of pancreatic digestive enzymes alongside imaging such as computer tomography (CT) [1]. CT scans can help predict the severity and clinical outcome of patients with acute pancreatitis by helping differentiate necrotic debris and other associated complications that might be present, such as a pancreatic fluid collection [1]. CT imaging, however, does not always yield a clear-cut diagnosis, with sensitivity ranging from 77 to 92% [1, 2]. This case demonstrates the unpredictable nature of a common condition and highlights the challenges in diagnosing the severity of acute pancreatitis and therefore the importance of maintaining a high level of clinical suspicion at all times. It demonstrates that severity scoring does not always correlate with subsequent clinical course. This case will be of value to all medical professionals, as it clearly illustrates the uncertain nature of acute pancreatitis and the vast array of sequelae that can arise. Unexpected consequences and surgical interventions may be prevented if a similar case presents in the future.
CASE PRESENTATION
A 69-year-old man was admitted to the emergency department with acute onset right-sided upper abdominal pain, with associated sweating and vomiting. On examination, he was tachycardic (heart rate 104), afebrile (temperature 36.8°C) and O2 saturations were 91% on 4 L of oxygen. There was voluntary guarding on

Contrast CT showing inflamed, enhancing pancreas (A) and the presence of paranephric fluid in the retroperitoneal region (B).
palpation of the epigastric region. No other systemic findings were noted at this time. Serum amylase was raised (727 U/L, normal range 30–110 U/L) [3]. Ultrasound of the abdomen revealed sludge within a thin-walled gallbladder and a diagnosis of acute pancreatitis secondary to gallstones was made. The patient’s severity stratification according to the Glasgow Criteria was 1, scoring only for age over 55 years [4].
Four days after admission, the patient complained of pain in his left lower abdominal quadrant. A tender, irreducible, erythematous swelling was apparent in the patient’s left groin. CT scans (Fig. 1) revealed extensive peripancreatic fluid with some infiltration of the left paracolic gutter, as well as extensive subcutaneous oedema and a small left inguinal hernia that did not contain any bowel loops (Fig. 2). The hernia became more painful and repeat CT scans showed a marked increase in the volume of fluid surrounding the pancreas and the degree of fluid tracking to the anterior and posterior paranephric spaces and left paracolic gutter was also greater than before.
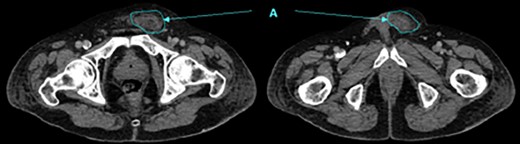
Contrast CT showing fluid tracking anteriorly into the left inguinal region (A).
A laparoscopic cholecystectomy and open hernia repair was planned. During surgery a pancreatic abscess was discovered with fluid tracking within the left inguinal canal. The left groin abscess was drained; however, the spermatic cord and cremaster were grossly implicated resulting in the need for a left orchidectomy. Post-operative CT scans showed a decrease in the inflammatory changes in the peripancreatic fat, in keeping with resolving pancreatitis.
DISCUSSION
This case of severe acute pancreatitis is incredibly rare. There have been no other published cases of patients undergoing an orchidectomy secondary to pancreatic fluid entering the inguinal canal. The differential diagnoses for a left-sided groin mass in males include femoral or inguinal hernia, epididymo-orchitis, lymphadenopathy or psoas abscess secondary to tuberculosis, pancreatic abscess, Hodgkin’s lymphoma, lipoma of the spermatic cord and perforation of the femoral artery or vein [5–7].
The clinical manifestations and underlying pathomorphologic events that occur along the natural course of acute pancreatitis can be divided into four, time-dependent entities [1]. Early complications of acute pancreatitis include interstitial oedema and necrotising pancreatitis, whereas later, less frequent consequences of acute pancreatitis include pancreatic pseudocyst and abscess formation [1].
In this patient, large retroperitoneal fluid collections of peripancreatic fluid developed over time and consequently tracked along the psoas muscle and entered the inguinal canal. Involvement of the inguinal canal and spermatic cord is an extremely rare complication of acute pancreatitis. Clinical signs included groin swelling and erythema, most likely due to irritation from necrotic debris with associated localised fat necrosis. The decision to intervene surgically and drain fluid in patients with acute pancreatitis is usually dependent on CT findings and clinical course; in this case, a diagnosis of an inguinal hernia was made from interpreting the CT. The patient was consented for inguinal hernia repair during which the presence of an unidentified pancreatic abscess with extension into the inguinal canal was incidentally found, resulting in surgical drainage and orchidectomy [1]. Currently, CT is the primary imaging modality to reliably diagnose and subsequently tailor management of acute pancreatitis [8]. CT is not only widely available but the literature sites specificity rates of ~100% and sensitivity rates between 77 and 92% [9, 10]. Despite this, we have illustrated a unique case with an outcome that was misdiagnosed radiologically. The case highlights the need for a high level of suspicion when making diagnoses in patients with acute pancreatitis, presenting with other abdominal symptoms. The case illustrates the array of complications that can arise along the natural course of a seemingly standard presentation of acute pancreatitis. It also presents the challenging nature of pre-determining the severity of a case of acute pancreatitis, despite using the Glasgow criteria and CT imaging, therefore demonstrating the importance of retaining a high level of clinical suspicion for patients with acute pancreatitis and associated obscure symptoms.
INFORMED CONSENT
The patient has consented for this case report to be published.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



