-
PDF
- Split View
-
Views
-
Cite
Cite
Rika Tobita, Ryota Nakamura, Yoshihisa Inage, Unusual pulmonary vein variant in a patient with right upper lobe lung cancer, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa113, https://doi.org/10.1093/jscr/rjaa113
Close - Share Icon Share
Abstract
It is essential to understand individual pulmonary anatomy, and the relationship between the tumor and surrounding organ, when lung resection is conducted. Recently, many anomalous pulmonary venous variations have been detected using three-dimensional computed tomography (3D-CT). Herein, we report the case of a 62-year-old women with lung cancer and an anomalous right upper lobe pulmonary vein that drained into the left atrium between the pulmonary artery and bronchus. Preoperative 3D-CT clearly demonstrated the anomalous pulmonary vein, and we safely performed lung resection by thoracoscopic surgery. Therefore, 3D-CT images can help ensure the safety of patients with aberrant vasculature during lung resection.
INTRODUCTION
As the proportion of video-assisted thoracoscopic surgery (VATS) increases for lung cancer, it is important to recognized individual anatomical pulmonary vessels accurately to avoid serious complications. With advances in imaging technology, it has become possible to obtain better information on vascular abnormalities. As a result, precise information about individual anatomical variations of the pulmonary vessels is available before surgery. In particular, preoperative three-dimensional computed tomography (3D-CT) images have provided accurate information on vascular abnormalities, and 3D-CT images can play an important role for VATS anatomical resection [1, 2].
The pulmonary venous drainage pattern of the right upper lobe is commonly anterior and caudal to the pulmonary artery, reaching the hilum. We report a case of surgically treated for right upper lobe lung cancer with a very rare variation of pulmonary venous anatomy. Using preoperative 3D-CT images, we could identify this venous drainage pattern that was located behind the main pulmonary artery and in front of the bronchus intermedius and we managed to safely perform lung resection under VATS.
CASE REPORT
A 62-year-old woman was referred to our hospital due to suspected lung cancer. The chest CT revealed a 32-mm solid pulmonary nodule in the right upper lobe without lymph node enlargement (Fig. 1). The 3D-CT revealed that the right upper pulmonary vein (V1 + 2) ran posterior to the pulmonary artery and anterior to the bronchus intermedius (Fig. 2A and B). On the other hand, anterior segmental vein (V3) had venous return anterior to the top of hilum. Based on this information, we performed right upper lobectomy with systemic lymph node dissection under VATS. Intraoperative findings showed that the V1 + 2 drained to the left atrium between the main pulmonary artery and the bronchus intermedius (Fig. 3), which was clearly detected by the preoperative 3D-CT. We exposed the pulmonary vessels at the hilum and V3 was found superiorly on the most ventral side of the hilum, whereas we could not identify V1 + 2, which is usually located anterior to the hilum. After the V3 and the ascending pulmonary artery were ligated, we recognized the V1 + 2 at the dorsal side of the main pulmonary artery. The anomalous V1 + 2 were isolated and ligated with a vascular stapler. Therefore, it was possible to complete VATS lobectomy without any complications. Pathological examination showed adenocarcinoma with no lymph node metastasis. The postoperative course was uneventful, and the patient was discharged on postoperative day 7.
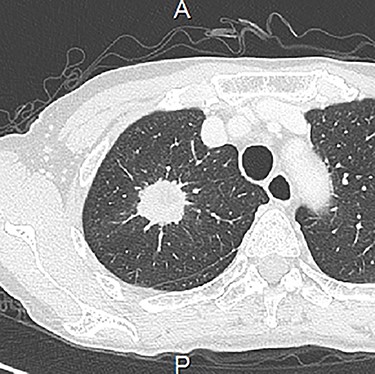
Chest CT showed a 32-mm diameter solid mass in the right upper lobe.
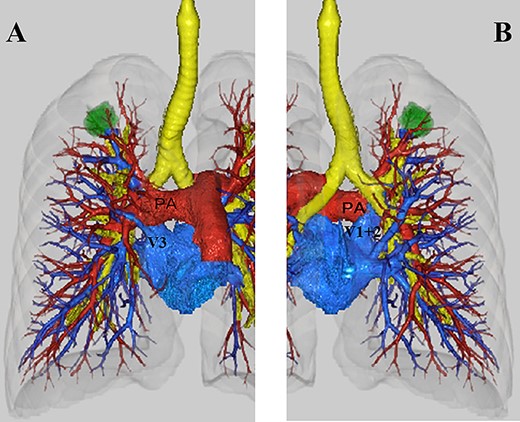
(A) Anterior view on three-dimensional computed tomography (3D-CT). V1 + 2 ran behind the pulmonary artery. V3 was located superiorly on the most ventral side of the hilum. (B) Posterior view on 3D-CT. V1 + 2 ran in front of the bronchus (PA: main pulmonary artery).
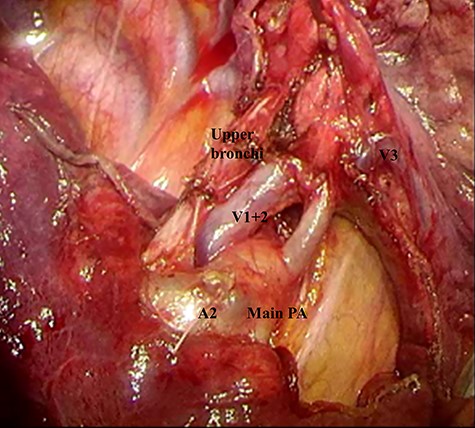
The operative findings in this patient after V3 and A2 ligation. V1 + 2 was recognized between the main pulmonary artery and the bronchus intermedius.
DISCUSSION
Several reports have focused on the variation and frequency of pulmonary venous variants, especially of the right upper pulmonary veins. Anatomical analysis of the human body using surgically resected specimens has been performed with two-dimensional (2D) images [3, 4]. Recently, pulmonary veins have been evaluated preoperatively using 3D-CT, and various drainage patterns have been identified. These reports concluded that 3D-CT was a useful tool for the evaluation of individual anatomical variations preoperatively for performing VATS [1, 2]. The frequency of abnormal pulmonary venous return in the right side (32.8%) is higher than that in the left side (2.6%), and anomalous venous return of right V2 is more common [2]. The right upper lobe pulmonary vein is usually located anterior to the hilum, and the pulmonary artery located just posterior to it. There have been several reports of the right upper lobe pulmonary vein which crossed posterior to the bronchus intermedius, [5] or which connected to the superior vena cava [6]. However, there have only been two cases reported with anomalous right upper lobe pulmonary vein located between the pulmonary artery and the bronchus [7, 8]. This vascular abnormality in one patient could not be detected on preoperative CT scan [7]. In another patient, the presence of the aberrant pulmonary vein was confirmed by preoperative 3D-CT [8]. The difference in the power of detecting abnormal pulmonary veins in these two patients was presumed to be due to technological advances. A recent report revealed that almost all of the pulmonary artery branches (97.8%) were accurately identified, and all anomalous arterial and venous branching patterns were precisely confirmed using 3D-CT [1]. This type of pulmonary vein variation presents a risk of pulmonary artery injury when surgeons divide the minor fissure anteriorly with a linear stapler because of a misunderstanding of pulmonary vein location. Furthermore, if surgeons misunderstand the middle lobe pulmonary vein, which was located superiorly on the ventral hilum as in this aberrant pattern, there will be a risk of additional resection during ligation of the upper pulmonary vein and the middle lobe vein.
VATS has been accepted as a standard surgical procedure for patients with lung cancer. However, it is necessary to confirm the pulmonary structure through a video camera in a 2D setting, and the VATS approach has a limited surgical field of view. Therefore, it is important to evaluate the pulmonary vessel pattern in each patient using preoperative 3D-CT to safely perform VATS lung resection. In our case, we clearly visualized this anomalous pulmonary vein using 3D-CT preoperatively, and we could avoid the risk of pulmonary artery injury due to a misunderstanding of the middle lobe vein. As a result, we safely performed VATS right upper lobectomy.
In conclusion, preoperative identification of this anomalous pulmonary vein using 3D-CT was very important to perform surgery correctly. Surgeons should keep in mind this anomalous pulmonary venous pattern. The 3D-CT images were useful in finding the aberrant vessels.
CONFLICT OF INTEREST STATEMENT
None declared.
Funding
None.



