-
PDF
- Split View
-
Views
-
Cite
Cite
Awadh Alqahtani, Emad Aljohani, Unusual presentation of rare complication following endoscopic gastroplasty: case report, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa184, https://doi.org/10.1093/jscr/rjaa184
Close - Share Icon Share
Abstract
A 35-years-old female post-endoscopic gastroplasty presented to the emergency department complaining of epigastric abdominal pain. The abdominal examination showed epigastric and tenderness. On abdomen computerized axial tomography (CAT) scan she had small bowel obstruction with twisting of mesenteric vessel. The patient taken to the operating room for diagnostic laparoscopy and proceed, laparoscopic examination showed proximal dilatation of small intestine with collapse of distal part of jejunum, the obstruction identified, as fibrous band originating from the stomach to the proximal part of jejunum, this band caused by suture penetrating the stomach wall, which is going with the previous history of the endoscopic gastroplasty, reduction of the internal hernia done by releasing of the fibrous band, the herniated segment was healthy. Internal hernia can present with variety of complications. To the best of our knowledge from the literature review, this is the first case to be reported as internal abdominal hernia secondary to endoscopic gastroplasty.
INTRODUCTION
The accelerating global obesity epidemic portends substantial increases in morbidity and mortality. This has critical economic implications, most obviously for future healthcare spending, but also in terms of economic productivity, disability and potential increased reliance on social safety nets. Bariatric surgery has been shown to be the most effective treatment, with the most significant weight loss and decrease in comorbidities, such as type 2 diabetes mellititus. It is logistically and economically not feasible to offer surgery to those who may benefit, with worldwide estimates of <1% of the population target having access to surgery [1]. For these reasons, less complex and possibly less expensive such as endoscopic therapies are appealing and could provide an opportunity to reach a greater number of patients, earlier in their onset of obesity, including those with body mass indices between 30 and 35 kg/m2 [2]. Internal hernia refers to the displacement of the abdominal internal organs from their original position through a normal or abnormal channel or fissure in the abdominal cavity to an abnormal cavity. The internal hernia is one of the uncommon causes of acute abdomen [3]. However, it is not previously mentioned in the literature that endoscopic gastroplasty to cause internal hernia. This paper reports a case of internal hernia with intestinal obstruction caused by endoscopic gastroplasty.
CASE REPORT
A 35-years-old female, 9 months post-endoscopic gastroplasty presented to the emergency department complaining of epigastric abdominal pain for 5 days, the pain is radiating to the umbilicus associated with nausea and vomiting. On general examination, she is vitally stable with HR 88 B/min, BP 116/66 and temperature 36.9°C, the abdominal examination showed epigastric and tenderness. On abdomen CAT scan, she had partial small bowel obstruction with adhesive band originating from the stomach (Fig. 1). Barium meal showed dilatation of the second part of duodenum due to band like structure (Fig. 2). The patient admitted to the hospital with a diagnosis of small bowel obstruction and kept NPO; Nil Per Os, on IV fluids and nasogastric tube drainage.

CAT scan showing partial small bowel obstruction with adhesive band originating from the stomach.
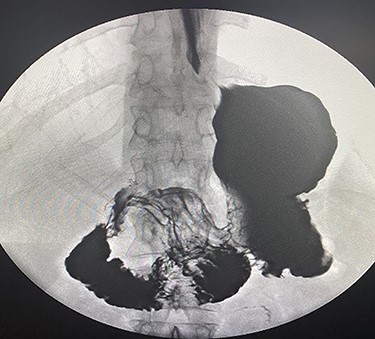
Barium meal showed dilatation of the second part of duodenum due to band like structure.
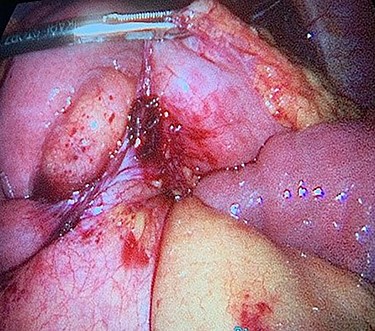
The patient taken to the operating room for diagnostic laparoscopy and proceed, after insufflating the abdomen the whole abdomen examined and showed proximal dilatation of small intestine with collapse of distal part of jejunum, the ileocecal junction identified and the small bowel examined proximally till the obstruction identified, which is fibrous band originating from the stomach to the proximal part of jejunum (Fig. 3), examination of this band showed that this band is caused by suture penetrating the stomach wall, which is going with the previous history of the endoscopic gastroplasty, reduction of the internal hernia done by releasing of the fibrous band, the herniated segment was healthy (Fig. 4).

Fibrous band originating from the stomach to the proximal part of jejunum.
DISCUSSION
Endoscopic sleeve gastroplasty (ESG) is an incisionless, minimally invasive technique, which has been developed for bariatric treatment. ESG is a safe and effective endoscopic bariatric procedure with generalizability and reproducibility. After the ESG the patient may complain of nausea and pain, both of which can be managed with a variety of medications. The severe adverse events that have been reported include leaks, perforation and bleeding (all < 2%) [4,5].
Complications due to internal hernias often require emergency abdominal surgery which is associated with significant morbidities and mortality. The most frequent manifestations include persistent progressive abdominal crampy pain, nausea, vomiting and abdominal distension. By the time patient develops, obvious signs of peritonitis such as rebound tenderness and rigidity, most of them have intestinal gangrene and intestinal perforation. Therefore, early diagnosis is the key in the management of intra-abdominal internal hernias.
Our patient had internal abdominal hernia secondary to adhesive band formed on the endoscopic gastroplasty suture. This complication was not expected preoperatively as it was not mentioned in the literature before nor listed in the known endoscopic gastroplasty complications.
Although endoscopic gastroplasty is a safe procedure for the obesity management, attention must be paid to the possibility of this extremely rare complication in patients who present with acute abdominal symptoms and a history of this surgical procedure. To the best of our knowledge from the literature review, this is the first case to be reported as internal abdominal hernia secondary to endoscopic gastroplasty.
FUNDING
None.
CONFLICT OF INTEREST STATEMENT
None declared.
ETHICS APPROVAL
Not applicable.



