-
PDF
- Split View
-
Views
-
Cite
Cite
Perçin Karakol, Melihcan Sezgiç, Burak Ergün Tatar, Caner Gelbal, Can Uslu, The use of dorsoradial forearm flap for the treatment of dorsal hand defect, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa153, https://doi.org/10.1093/jscr/rjaa153
Close - Share Icon Share
Abstract
Generally dorsal hand defects are often closed with a flap. Dorsoradial forearm artery flap has generally been used in thumb defects; however, it can also be used in the reconstruction of dorsal hand defects thanks to its wide rotation arc and appropriate pedicle length. In this case report, we presented the outcome of a case where the dorsoradial forearm flap was applied to treat the dorsal hand defect. A 27-year-old patient was admitted to emergency room with trauma on hand. Fixation of metacarpal bone fractures was performed. The dorsoradial forearm flap was elevated and inserted in order to close an opening exposing bones and tendons in the dorsum of hand. There was no complication with flap viability in the postoperative period. Patient’s joint range of motion and vital functions were acceptable. Dorsoradial forearm flap, which is generally used in thumb reconstruction, can also be used in dorsal hand defects.
Introduction
The dorsum is a particular area of the hand due to thin skin and the absence of subcutaneous fatty tissue. Tendon, nerve or osseous structures may be exposed as a result of various types of injuries. Different methods can be used for reconstruction, including regional pedicled flaps to free flaps [1–4].
Although these flaps are frequently used, most of them are too bulky for relatively small defects and generally show donor site morbidity.
The dorsoradial flap (DRF) defined by Bakhach et al. has generally been used in the dorsal thumb defects as well as being used in the dorsal hand defects [5]. The dorsoradial forearm flap is a cutaneous flap with a dorsoradial artery pedicle [6]. The pivot point of the pedicle provides the flap with a rotational arch wide enough to cover the dorsal defects of the thumb and hand and even the palmar defects of the wrist [7]. Although several publications have reported the application of the DRF in the dorsal defects of the thumb, few reports described its use in the dorsal defects of the hand.
In this case report, we have described the application of DRF for a dorsal defect that exposed bones and tendons following the reconstruction of metacarpal fractures in fingers due to a blunt trauma on the right hand.
Case report
A 27-year-old male was admitted to the emergency room after blunt trauma on the dorsum of the right hand. In his physical examination, circulation and sensory findings were normal, but the motor functions were limited. On the X-ray radiograph, metacarpal base fractures were detected in the index, middle and ring fingers (Figs 1 and 2). After the surgical area was sterilized, the dissection was initiated under tourniquet and general anesthesia. Tendons were found to be intact due to blunt trauma, and the metacarpal base fractures in fingers were exposed (Fig. 3). These bones were stabilized with Kirschner wires (Fig. 4). After the debridement of dead tissues and opening the tourniquet, bleeding was controlled, and skin was stapled. The flap was planned for the 2 x 2 cm defect, which corresponds to the third metacarpal bone and exposed the tendon and bone (Fig. 5). The first dorsal metacarpal artery (FDMA) flap was initially considered; however, a dorsoradial artery flap was preferred since the dissection reached to the second metacarpal bone.


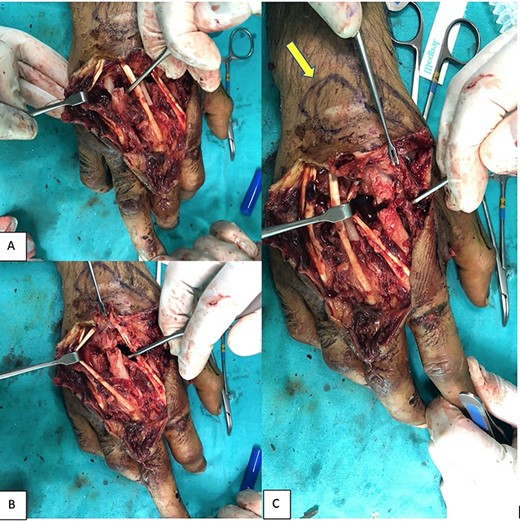
Exposing the metacarpal fractures. In the second (C), third (B) and fourth (A) fingers and intact tendons. Flap marking intraoperatively: yellow arrow.


A skin island was drawn with a skin marker on the distal part of the forearm, and the flow was measured with Doppler ultrasonography from the medial of the Extensor Pollicis Longus (EPL) tendon in the pedicle. The incision was initiated proximally under tourniquet; the distal forearm fascia was included in the flap, which was elevated above the extensor retinaculum; the medial branch of the radial nerve was identified and protected. The EPL and Extensor Carpi Radialis Longus (ECRL) tendons at the level of the distal dorsal retinaculum were identified and retracted; the dissection was deepened; skin incision was introduced onto the pedicle preserving the superficial venous network; and the dissection was continued meticulously up to the apex of the first intermetacarpal space to allow a rotation that permitted insertion to the defect area. Tourniquet was opened, and bleeding was controlled; the flow in the pedicle was measured with Doppler ultrasonography. The donor area was closed with primary closure and the operation was terminated (Fig. 6).

The flap inset. Yellow arrow: donor site closed with primary closure.
No postoperative complications were observed; K-wires were removed in the fourth week. No problems were encountered during wound healing (Figs 7 and 8). Hand movements have reached the level sufficient to maintain vital functions after intensive physical therapy.


Discussion
The reconstruction of dorsal hand defects is critical for hand mobility and function. Several methods of reconstruction have been described, varying from skin grafts to free flaps. Skin grafts are not used for defects with tendon or bone exposures, and the secondary contraction is a significant disadvantage in suitable cases where they are used [8].
Pedicled groin flaps were used quite frequently in the past. However, prolonged immobilization resulted in a need to use the groin flaps as free flaps. Although the radial forearm flap (RFF) was frequently used to cover large defects in the past, the frequency of its use has decreased in time due to the sacrification of major arteries and donor site morbidity. The posterior interosseous artery (PIA) flap, which was first defined by Zancolli et al. is used for the reconstruction of dorsal hand defects in the pedicle and free forms [9]. PIA has the advantages of major arterial preservation, robust blood flow and reduced donor site morbidity but the increased frequency of venous congestion is a significant disadvantage [8].
Ulnar and radial forearm perforator flaps can be used as fasciocutaneous or adipofascial flaps. Their use is limited in the reconstruction of distal defects because the pedicles are very proximal. Besides, their dissection is relatively more difficult.
The RA passes the FDMA and dorsoradial artery and enters the volar side of the hand at the level of the first web space. The FDMA flaps, first described by Foucher and Braun [10], are used in dorsal or oblique thumb defects. The DRF has two variants based on the separation from the RA. In type-1 DRF (84%), the DRA exits directly from the RA 3–4 mm proximal to the FDMA; in type-2 DRF (16%), both FDMA and DRA exit from a common trunk. It should be noted that these variations do not change the flap elevation and use. The DRF is more advantageous than the RFF due to the absence of major arterial sacrification, than the PIA flap since it is not bulky and than the perforating flaps due to the relative ease of dissection and wide rotation arc. It is a disadvantage that it is not a sensory flap [7]. Although the DRF is generally used as a fasciocutaneous flap, it can also be used as a chimeric flap in which secondary metacarpal bone is included.
This case report has demonstrated that, in addition to other reconstruction methods, the Dorsoradial Forearm flap (DRF) can also be used in dorsal hand defects.
ACKNOWLEDGEMENTS
There is no contributor who does not meet the criteria for authorship. Hence, the section of acknowledgement is none.
Conflict of interest statement
None declared.



