-
PDF
- Split View
-
Views
-
Cite
Cite
Shannon Caesar-Peterson, Katrina Tulla, Colton Southall, Ying Lin, Elvita Genelus-Dominique, A rare case of signet ring cell carcinoma of the appendix, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa139, https://doi.org/10.1093/jscr/rjaa139
Close - Share Icon Share
Abstract
Primary appendiceal carcinoma itself comprises less than 0.5% of all gastrointestinal malignant neoplasms. However, signet ring cell carcinoma of the appendix is an extremely rare subset of primary appendiceal carcinomas. This sub-type of appendiceal carcinoma represents only 4% of all appendiceal carcinomas. In this case report, we present a case of signet ring cell carcinoma found in a 65-year-old male patient which presented as acute appendicitis. He was diagnosed after a laparoscopic appendectomy by histopathological evaluation.
INTRODUCTION
The main types of appendiceal carcinomas include neuroendocrine (previously called carcinoid), adenocarcinomas, adenocarcinoids and signet-ring cell carcinomas [1–3]. A primary signet ring cell carcinoma of the appendix is a rare phenomenon of surgical practice since it can mimic and present as a routine acute appendicitis, ovarian torsion and other right lower quadrant pathologies [4]. Therefore, it is difficult to diagnose and needs histopathological evaluation after the procedure by the clinical and surgical pathologist [1]. It was first described in 1969 by having both neuroendocrine and glandular differentiation and this therefore offsets it from the other types of appendiceal carcinomas making it an extremely rare primary cancer [5]. It most likely originates from pluripotent intestinal crypt epithelial stem cells as well as loss of the tumor suppressor, Notch [6]. It is also noted that mucin droplets and neuroendocrine secretory granules are present in these epithelial intestinal crypts that help form the tumor [5]. Appendectomy is the treatment of choice followed by superimposed right hemicolectomy and adjuvant chemotherapy if warranted from perforation or invasion of location structures [7].

CT scan shows acute appendicitis. Dilated fluid-filled appendix measuring up to 2.4 cm in diameter × 8.3 cm in length with periappendiceal inflammation ((A) Coronal view, (B) sagittal view, (C) axillary view).
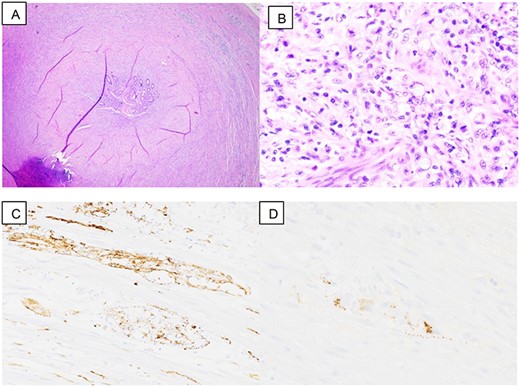
Pathology slides are: (A) low power view: appendix with thicken wall, (B) high power view: signet ring cell, (C) synaptophysin stain: positive and (D) chromogranin stain: focally positive.
CASE REPORT
A 65-year-old male patient with a pertinent past medical history of hypertension, type 2 diabetes mellitus, alcohol and tobacco use presented with right-sided abdominal pain. The patient stated that the pain started 3 days prior, with a previous hospital visit the day before but the patient left against medical advice. The patient described the pain as sharp, intermittent, 8/10 and constant. He denied any fever, chills, nausea, vomiting, diarrhea, dysuria, any significant weight loss, changes in bowel habit or previous colonoscopy. His vital signs on presentation were temperature of 98.9°C, heart rate of 101 bpm, respiratory rate of 16 breaths/min, blood pressure of 117/68 mmHg and oxygen saturation rate of 95% on room air. On focused physical examination, the abdomen was tender to deep palpation in the right lower quadrant with a negative Rovsing’s sign, no rebound and no guarding, which correlates with a clinical diagnosis of acute appendicitis. Imaging showed a dilated fluid-filled appendix measuring up to 2.4 cm in diameter × 8.3 cm in length with periappendiceal inflammation as well as a trace left hydroureter and a non-obstructing right renal calculus. On admission, the patient had leukocytosis of 11.5 with a differential of 75.7% neutrophils and 14.5% lymphocytes. Patient was placed on intravenous antibiotics (Zosyn) and taken for laparoscopic appendectomy.
During surgery, the appendix was noted to be adhered to the abdominal wall and multiple adhesions to the surround mesentery at the base of the appendix. The appendix measured 10.5 cm in length × 1–2 cm in diameter when it was extracted and sent to pathology (Fig. 1). The serosa of the appendix was dull and hemorrhagic. There was a firm area measuring 2.5 cm at the base. On pathology, the cuts revealed a gray white homogeneous appearing tumor measuring 2.5 × 0.7 × 1.3 cm located at the proximal appendix with positive lymphovascular invasion (T3, NX, MX). Pathology results showed carcinoma of ex-goblet cell carcinoid, signet ring cell type (Fig. 2). Microscopic findings indicated the involvement of muscularis propria into subserosa of mesoappendix with the absence of tumor perforation. Immunohistochemical staining revealed positive staining for chromogranin and synaptophysin, supporting the diagnosis (Fig. 2).
Patient tolerated the procedure well and was kept on intravenous zosyn for 3 days then discharged with oral keflex to complete a 7-day course. Post-operatively, the patient was lost to follow up although several attempts were made to contact the patient.
DISCUSSION
Appendiceal carcinomas are difficult to diagnose preoperatively or perioperatively due to its rare incidence and classic presentation of acute appendicitis [3]. As in this case, the patient presented with right-sided abdominal pain and denied any major unintentional weight loss, changes in his recent appetite or any recent illnesses. There was careful clinical and surgical histopathological eva luation of the appendiceal tumor to bring about the diagnosis.
The mean average age for this specific type of appendiceal carcinoma is 62 years old and has a propensity for those who are Caucasain, with a male to female ratio of 1:11. To further support a diagnosis, the immunohistochemical staining is of vital importance; in our case, it was chromogranin and synaptophysin positive. Another important stain that is specific for signet ring cell carcinoma is CDX-2, caudal-type homeobox transcription factor 2, marker, but that was not available for this case [1, 6].
Goblet cell-type carcinomas are typically more aggressive, and signet ring cell classification is ‘defined as goblet cells or signet ring cells arranged in irregular large clusters, with the lack of confluent sheets of cells in a discohesive single file or single cell infiltrating pattern with significant cytologic atypia, and desmoplasia and associated destruction of the appendiceal wall’ [7]. The 5-year survival rate is 20.5% and will drop to 6.7–14% if there is diffuse peritoneal metastasis [1]. Since this tumor is morphologically and immunohistochemically different from all other appendiceal carcinomas, it is important that the entire appendix be removed at time of surgery because the morphology is prognostically important and prefers to make peritoneal folds and spread on the surface [5]. Follow-up for recurrence is important since it is a neuroendocrine-based tumor.
In conclusion, a signet ring cell carcinoma of the appendix is extremely rare. It is presentation mimics acute appendicitis and other right lower quadrant surgical pathologies, making it a hidden wonder. Only upon surgical intervention with subsequent pathological evaluation, will the diagnosis of signet ring cell or ex-goblet cell carcinoma of the appendix be made. Grading and staging are important for treatment and warranting further surgery in the form of right hemicolectomy and further treatment with adjuvant chemotherapy. Since these tumors are aggressive, lifelong follow-ups are recommended for recurrence.
ACKNOWLEDGEMENTS
We would like to thank the department of pathology at wyckoff for the slides provided for this figure.



