-
PDF
- Split View
-
Views
-
Cite
Cite
Farah Mohanna, Anas Slaibi, Zuheir Al-Shehabi, Moufid Mahfoud, Osteosarcoma of the frontal bone: a study of a rare case in a 17-year-old female, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa138, https://doi.org/10.1093/jscr/rjaa138
Close - Share Icon Share
Abstract
Head and neck osteosarcomas are infrequent and usually present in the third–fourth decades of life. However, they are extremely rare in the pediatric population. Primary involvement of the cranial vault, excluding the mandible and maxilla, is an exceedingly rare phenomenon; thus, the number of clinical studies published in the literature is limited. Because of the anatomy of the head, complete resection may be difficult to achieve. Furthermore, an aggressive surgical approach can cause a significant functional impairment or cosmetic defect. We report the case of a 17-year-old patient with an aggressive recurrence of multiple tumors in the left side of the skull accompanied with a severe headache and complete left-sided vision loss with no metastases at presentation. The recurrence of the tumor was preceded by pregnancy and delivery, which raised the question of whether pregnancy hormones were a provoking factor in the recurrence of the tumor or not.
INTRODUCTION
Primary osteosarcoma of the skull is rare, with an incidence of only 1–2% of all skull tumors. Only fewer than 150 cases have been reported. Reports on the cases of primary pediatric osteosarcoma of the skull are scarce, accounting for approximately 15 cases [1]. Approximately 6% of osteosarcomas occur in the head and neck region, with the majority occurring in the mandible [2]. The majority of osteosarcomas occur without a familial predisposition or a history of exposure to radiation [3]. Due to its rarity, treatment of such cases, especially in children, can be tricky as there are not enough clear guidelines on how to manage it. Herein, we report a case of osteosarcoma of the left parietal bone and describe the radiological features, clinical symptoms and the treatment outcome using surgical resection and radiotherapy.
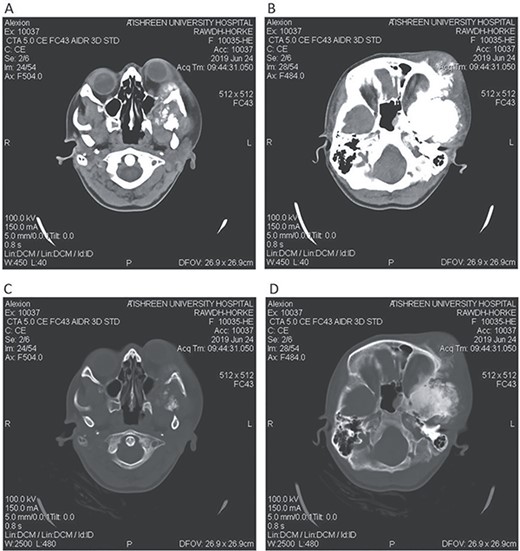
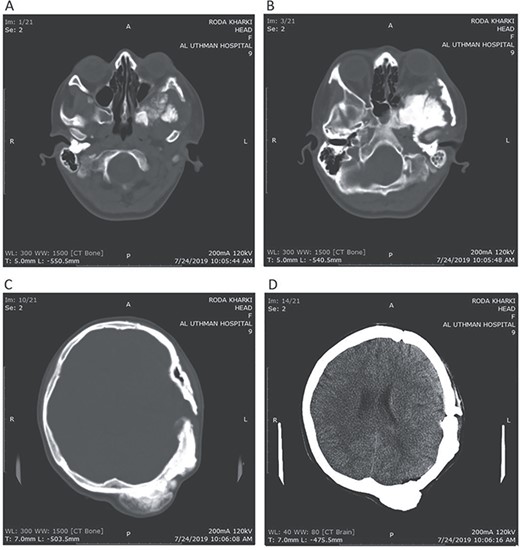
CT head tissue window (A, B). A. Invasion of the maxillary sinus and orbit. B. Invasion of the parietal, temporal and frontal lobes. A remarkable exophthalmos. Bone window (C, D). C. The bone-forming lesion showing the same density of the bone. D. Invasion of the sphenoid, temporal and parietal bones.
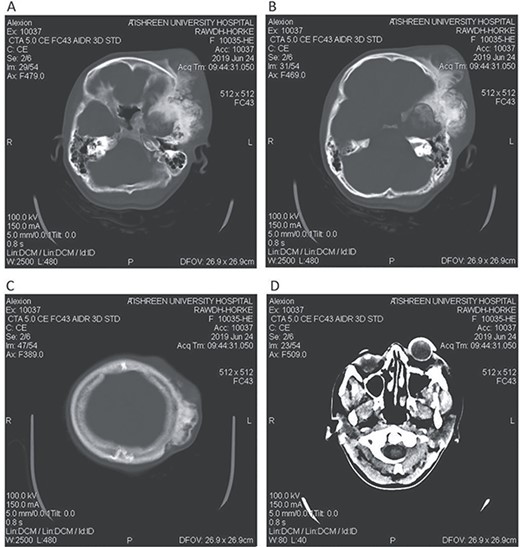
CT head bone window (A–C). A. Invasion of the frontal bone. B. Invasion of the orbit. C. Invasion of the parietal bone. D. Invasion of the sphenoid, temporal and parietal bones.
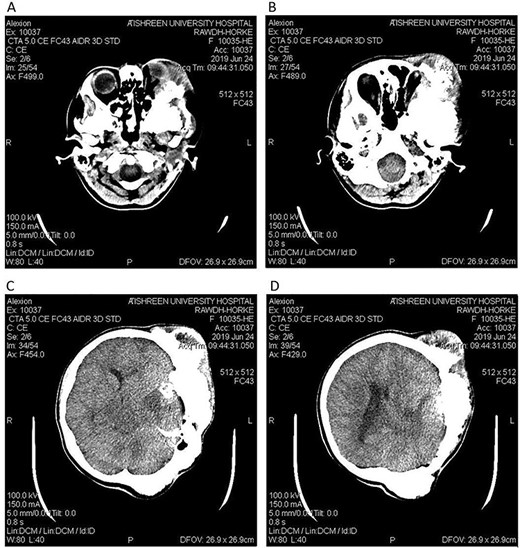
CT head tissue window. A, B. Invasion and destruction of the surrounding tissue. C. Minor shift of the elements of the midline to the right side due to the edema. D. The edema applies pressure to the left lateral ventricle.
CASE PRESENTATION
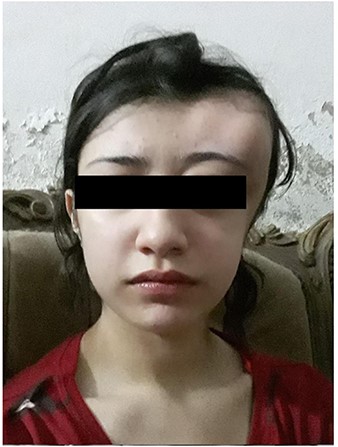
A 17-year-old female presented with a history of osteosarcoma that was confirmed after undergoing a surgery to remove an enlarging bone tumor in the left temporal region 2 years ago. She later got pregnant and delivered her child but never got back for a checkup until she was admitted to our hospital with a severe and unresponsive to medication headache that progressed over the course of 6 months and blurred vision that progressed to complete left-sided vision loss. Physical examination revealed a tough and mobile yet fixed at the base 7-cm mass towards the left of the frontal bone. Many more masses were revealed in the left side of the skull including the anterior cranial fossa, orbit, base of the skull and the left part of the occipital region where the previous procedure was performed (Fig. 1). These masses had been increasing in size probably under the influence of pregnancy hormones causing pain that radiated along the orbital and maxillary branches of the left trigeminal nerve. Physical examination and past medical history were otherwise unremarkable. Laboratory tests were all normal, and her family history was negative. Staging studies showed no evidence of distant metastatic disease in the chest, the abdomen and the pelvis. CT scan of the skull revealed a bone-forming non-lytic lesion accompanied by periosteal reaction. This lesion bulges to the outside towards the scalp spreading into both the soft tissues and the inside of the entire left side of the skull with a sunburst-pattern (Figs 2 and 3). Its rims are unsymmetrical and pointy, and it bulges into the left orbit outside the muscles causing exophthalmos with a semi-complete proptosis of the eyeball out of the orbit (Figs 2 and 3). This lesion applies pressure to the left frontal and temporal lobes causing mild edema in both these lobes without invading the brain tissue. This edema in turn applies pressure to the left lateral ventricles (minor shift of the elements of the midline to the right side can be seen on CT) (Fig. 4). Due to the tumor’s wide spread, the surgical procedure was performed in two stages (approximately 6-hour-long each). In the first stage, the bone mass was removed through a procedure of wide skull approach including the frontal, temporal and parietal bones and a removal of the invading part of the temporal muscle. Moreover, the lateral wall and roof of the left orbit were removed, the left optic nerve was dissected free and part of the meninges was removed and replaced with an autogenic patch from the fascia lata. Then, the bone loss was compensated for by using bone cement Synicem VTP (poly methyl methacrylate and Barium sulfate), and the orbit was rebuilt; the eyeball was placed back with noticeable decline of the exophthalmos. In the second stage, a complementary left parietal occipital incision of the previous approach was performed 3 weeks later; the remaining of the frontal and occipital bones was removed, and a partial mastoid surgery was done. Furthermore, the cavernous sinus were revealed and found to be not invaded. Later on, the normal skull shape was restored using the same cement. The histopathology of the lesion revealed proliferation of neoplastic chondroblasts, osteoblasts and spindle-shaped cells. The features are consistent with low-grade chondroblastic osteosarcoma (Fig. 5). The patient did not need ICU admission. She recovered well 3 days after the surgery and was discharged with no deficits. A CT scan that was performed post-operatively revealed that the masses were successfully excised (Figs 6 and 7). At the last follow-up 1 month post-operation, the patient was scheduled to undergo a course of radiotherapy, 60 Gy of radiotherapy in 30 fractions over 4 weeks without chemotherapy, as it is not recommended with low-grade osteosarcoma.
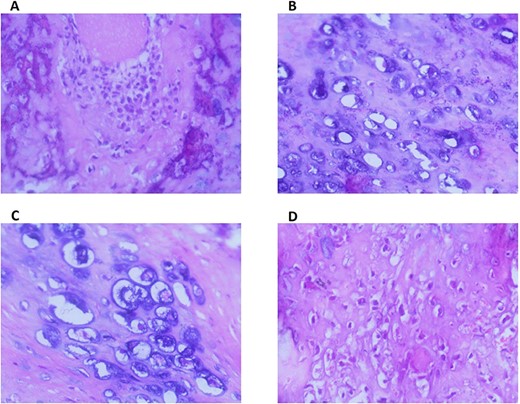
A. Low-power magnification of the tumor showing proliferation of chondroid tissue with scattered areas of osseous differentiation. (H&E stain, ×100). B. The chondroid matrix exhibiting atypical chondroblasts and chondrocytes with large pleomorphic nuclei and prominent nucleoli (H&E stain,×200). C. The tumor cells are present in lacunar spaces. The periphery of the cartilaginous area (lower left) shows spindling of the tumor cells (H&E stain, ×400). D. Presence of epitheliod and spindle neoplastic osteoblasts with large hyper chromatic nuclei and few mitotic figures. (H&E stain, ×200).
DISCUSSION
Osteosarcoma is a tumor characterized by the production of osteoid by malignant cells, which primarily affects the long bones, particularly after radiation or chemotherapy for other neoplasms; however, 6–7% present in the head and neck [4]. The exact cause of osteosarcoma remains unknown; however, a number of risk factors have been identified. These include: bone dysplasias including Paget’s disease, fibrous dysplasia, enchondromatosis and hereditary multiple exostoses in addition to Li–Fraumeni syndrome (germ line TP53 mutation), retinoblastoma and Rothmund–Thomson syndrome. The only known environmental risk factor is exposure to radiation [3]. The clinical symptoms of primary skull osteosarcoma vary depending on the tumor site [5]. Unlike extremity tumors, skull osteosarcomas are often painless [5]. These patients frequently present with headaches, cranial nerve palsies, exophthalmos, visual impairments or increased intracranial pressure [5]. Generally, osteosarcoma appears as a bone-forming or lytic lesion; however, in our case, it is limited to the bone-forming type. Although the methods of treatment are widely varied, surgical resection is still the mainstream [6]. Complete surgical excision and wide surgical margins have been associated with improved survival; however, some studies have reported that chemotherapy increased survival rates by 5 years for patients with localized tumors from 20% to 60–70% [4, 7]. Nonetheless, low-grade osteosarcoma can be treated with wide resection without chemotherapy [8, 7]. The occurrence of cancer in a pregnant woman is a relatively infrequent event, with an incidence of 0.07–0.1% of all pregnancies. The influence of pregnancy on the initiation, promotion and development of sarcomas is yet unclear. It has been suggested that the hormonal, physiological and the mechanical changes during or after pregnancy and labor promote the process of malignancy and metastasis [9].
Postoperative CT head bone window (A–C). A. Regression of the pressure on the maxillary sinus. B. Decline of the exophthalmos. C. The parietal bone after excision of the masses. Tissue window (D). Regression of the pressure on left lateral ventricle and decline of the midline shift.

ACKNOWLEDGEMENTS
All thanks go to Zeinab Mohanna, an English Literature student in Tishreen University, for her linguistic revision and editing of our case and to Dr Azzam al-Armani for his radiology consult.
Funding
Self funded.
Conflict of interest statement
The authors have no conflict of interest to declare.



