-
PDF
- Split View
-
Views
-
Cite
Cite
Aqdas A Al Omran, Arwa H Ibrahim, Ameera S Balhareth, Chilaiditi syndrome: an unusual presentation in elderly man, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa141, https://doi.org/10.1093/jscr/rjaa141
Close - Share Icon Share
Abstract
Chilaiditi syndrome is a radiological manifestation of a large bowel interposition between the liver and right hemidiaphragm that associated with gastrointestinal symptoms. We report a case of 78-year-old Saudi male with multiple comorbidities, presented to the emergency department with two episodes of passaging a large amount of fresh, bright blood per rectum. Later, the patient was diagnosed with Chilaiditi syndrome and managed with conservative measures. The presence of Chilaiditi signs can be caused by an abnormality of either liver, colon or right hemidiaphragm that leads to sub-diaphragmatic space enlargement or intestinal hypermobility. Computed tomography imaging is the best diagnostic modality. Conservative treatment is the first line in management.
INTRODUCTION
Chilaiditi sign is a radiological finding of a large bowel interposition between the liver and right hemidiaphragm [1]. It can be symptomatic or asymptomatic; when the patient is having complaint, it is called Chilaiditi syndrome [1]. Caution must be taken, as this can be easily mistaken with pneumoperitoneum that considered one of the surgical emergencies when it is secondary to viscous perforation [1].
CASE REPORT
A 78-year-old Saudi male with multiple comorbidities including an old stroke resulted in a residual deficit, presented to the emergency department with the passage of a large amount of fresh, bright blood per rectum, two times before presentation; abdominal pain could not be assessed due to inability to communicate verbally, no nausea, vomiting or similar presentation previously. Recently, the patient was admitted as a case of bowel obstruction, which treated conservatively using a rectal tube and laxative.
Upon examination, the patient was conscious, alert, oriented to time place and person, not in respiratory distress. He was vitally stable except for hypotension (90/60 mmHg). The abdomen was soft and lax, distended, tympanic and no tenderness, with normal active bowel sound. Rectal examination showed the presence of fresh blood in the diaper, posterior anal fissure, and 11 o’clock external hemorrhoid.
Laboratory workup showed low hemoglobin: 7.9 (patient baseline 11), white blood counts: 9.6, platelet: 345, creatinine: 102, BUN: 11.1, sodium: 149 (high) and potassium: 2.6 (low). Coagulation profile (high): PT: 14.2, PTT: 33 and INR: 1.4.
Chest X-Ray was unremarkable except for the visualized part of the abdomen that demonstrates distended bowel filled with gases (Fig. 1).
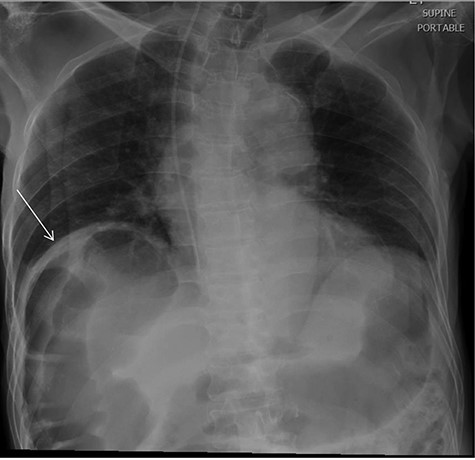
chest X-ray revealed visualized part of the abdomen demonstrate distended bowel filled with gases under the right hemidiaphragm.
Computed tomography (CT) chest abdomen pelvis with contrast indicated Chilaiditi sign (Fig. 2), large bowel obstruction at the recto-sigmoid junction, colonic diverticulosis, wall thickening at the proximal sigmoid/distal-descending colon and multiple foci of active rectal bleeding.
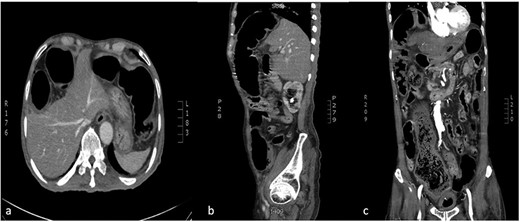
CT abdomen (a:axial) (b:sagittal) (c:coronal): transposition of a large bowel loop between the right hemidiaphragm and liver denoting Chilaiditi sign.
Sigmoidoscopy revealed old clotted blood, nodular anorectal ulceration, internal hemorrhoid and diverticulum without active bleeding. A biopsy was taken from anorectal ulceration showed: focal ulceration with focal hyperplastic changes, no evidence of dysplasia or malignancy.
Based on the previously mentioned investigations, the diagnosis of Chilaiditi syndrome was established. During the hospital course, the patient was managed conservatively via electrolyte correction, fluid resuscitation, blood transfusion and restrict oral intake.
DISCUSSION
Chilaiditi’s sign, firstly, observed by Cantini in 1865 then named in reference to Demetrious Chilaiditi, who reported three cases of an incidental radiological finding of large bowel interposition between the liver and right hemidiaphragm in 1910 [2, 10]. Estimated incidence has proved the rarity of this condition that ranges from 0.025 to 0.28% worldwide with 4:1: male-to-female ratio [2, 7].
Chilaiditi syndrome refers to the medical condition in which a Chilaiditi sign is accompanied by clinical symptoms [1, 8]. Generally, patients are asymptomatic, but non-specific gastrointestinal symptoms such as abdominal pain, nausea, vomiting, distension and constipation can present [1, 8]. Furthermore, other non-gastrointestinal symptoms can be encountered, such as right shoulder pain referred from diaphragmatic irritation [2].
Chilaiditi can be caused by an abnormality of either liver, colon or right hemidiaphragm. The small liver as in cirrhotic liver and post-hepatectomy, laxity of the suspensory ligaments, colonic hypermotility, high diaphragm secondary to muscular degeneration, or phrenic nerve injury; are all predisposing factors that will leave a chance for the colon to take place under the diaphragm [3]. Recently, Chilaiditi sign has been reported as post-procedural findings such as: colonoscopy, bariatric surgery and feeding tube insertion [3–5]. Adhesions as one of the commonest complications after surgical procedures will aggravate the condition if it is formed between the right organs, facilitating the colon’s interposition with the support of its fibrous tissue bands [9].
Early recognition of Chilaiditi syndrome is beneficial as this rare entity can cause confusion and mislead with pneumoperitoneum that considered as a surgical emergency, which will lead to unnecessary surgical interventions [9]. On the other hand, late identification of Chilaiditi syndrome is a disaster as it can lead to significant consequences such as volvulus, perforation and bowel obstruction [9]. While plain abdominal radiograph may help to differentiate between true pneumoperitoneum and Chilaiditi’s sign ‘pseudo-pneumoperitoneum’ by acquiring left lateral decubitus view revealing colonic haustra under the right hemidiaphragm, CT scan is proven to be diagnostic [2, 6].
Usually, the first line of treatment is conservative, including bed rest, IV fluids, NGT decompression and laxatives, unless the patient does not respond to initial conservative management or complications developed such as cecal volvulus, gangrene or perforation then surgical intervention is indicated [2]. Surgical intervention varies from simple colonoscopic reduction, colopexy for cecal volvulus to colonic resection if gangrene or perforation presents [2].
Unexpectedly, in this case, the patient did not seem to have any of the previously mentioned risk factors or causes. Therefore, this raises the concern for an incidental finding of Chilaiditi signs in older patients with unremarkable predisposing factors for such finding [2, 9].
CONCLUSION
In conclusion, Chilaiditi syndrome is a rare clinical presentation worldwide; however, it can be kept in mind once suspecting pneumoperitoneum as a sign in a chest X-ray. As CT is the diagnostic of choice for Chilaiditi sign, it should be ordered to minimize the incidence of unnecessary surgical intervention.
CONFLICTS OF INTEREST
There are no conflicts of interest.



