-
PDF
- Split View
-
Views
-
Cite
Cite
Saifullah Mohamed, Akshay J Patel, Yassir H Iqbal, Aaron Ranasinghe, Delayed presentation of a traumatic descending thoracic aorta aneurysm as an aorto-oesophageal fistula, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa135, https://doi.org/10.1093/jscr/rjaa135
Close - Share Icon Share
Abstract
Aorto-oesophageal fistula is a rarely described but life-threatening complication presenting with upper gastrointestinal haemorrhage. We present a case of a 58-year-old gentleman who presented to a peripheral hospital with a short duration of haematemesis and melaena and recent onset symptoms of dysphagia. This gentleman had a past medical history of alcohol excess and a history of trauma following a road traffic accident 38 years ago. Initial computer tomography scan demonstrated a large saccular aneurysm arising from the descending thoracic aorta adjacent to the oesophagus. The patient underwent radiological stenting of the large aneurysm with thoracic endovascular aortic replacement procedure. Follow-up computerized tomography (CT) angiography demonstrated satisfactory appearances of the thoracic aortic stent graft with no evidence of endo-leak. The triad of dysphagia, occult gastrointestinal blood loss and CT findings of a large aneurysm should prompt diagnosis or aorto-oesophageal fistula until proven otherwise.
INTRODUCTION
Aorto-oesophageal fistula is a rarely described but life-threatening complication presenting with upper gastrointestinal haemorrhage. It is often insidious in onset and has a high mortality but can be managed effectively if identified promptly [1]. The causes are multifactorial and it arises as a direct communication between the oesophagus and thoracic aorta leading to catastrophic haemorrhage. Management options initially involve resuscitation, stabilization, identification of cause and initial management, which can be definitive, or as a bridge to surgery. Thoracic endovascular aortic replacement (TEVAR) has been described for managing this complex condition with mixed results [2–4]. The prognosis of this condition is poor often due to the requirement of oesophageal procedure once the fistulous communication has been addressed. Sepsis due to infections and re-rupture is often ensuing sequelae. Spontaneous aorto-oesophageal fistula following previous history of trauma causing an undiagnosed aortic injury is rare.
CASE DISCUSSION
We present a case of a 58-year-old gentleman who presented to a peripheral hospital with a short duration of haematemesis and melaena and recent onset symptoms of dysphagia. This gentleman had a past medical history of alcohol excess and a history of trauma following a road traffic accident 38 years ago. The patient had no other risk factors or family history of aortopathy.
Initial basic investigations demonstrated a fall in his haemoglobin consistent with his history from 14 to 8 g/dl. Oesophago-gastro-duodenoscopy performed at the peripheral hospital was suggestive of a large Mallory–Weiss tear which was injected with adrenaline. Patient also underwent a computer tomography scan which demonstrated a large saccular aneurysm arising from the descending thoracic aorta adjacent to the oesophagus with secondary compression and displacement without any inflammatory or infective features (Fig. 1). CT aortogram did not demonstrate any contrast extravasation or blush into the oesophagus, but a fistula could not be excluded. Upon review of the imaging, it was decided that the patient should be transferred to our tertiary institution for further management with a probable diagnosis of aorto-oesophageal fistula.
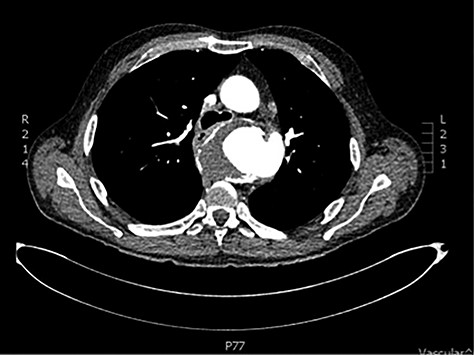
CT scan demonstrating close relationship of oesophagus and aortic aneurysm sac.
The patient was transferred and stabilized on the critical care unit and discussed with the interventional radiologist. In conjunction with the interventional radiologist and cardiothoracic teams, the patient underwent radiological stenting of the large aneurysm with TEVAR procedure (Figs 2 and 3). Following the procedure, the patient continued to have large volume haematemesis and melaena and underwent repeat oesophago-gastro-duodenoscopy which demonstrated large amount of blood and clot in the distal oesophagus and stomach with continuous brisk active arterial bleeding at approximately 40 cm, which was unsuitable for any endoscopic therapy. Follow-up CT angiography demonstrated satisfactory appearances of the thoracic aortic stent graft with no evidence of endo-leak. The left subclavian artery was well opacified, and the excluded aneurysm sac contained multiple locules of gas suspicious of ongoing fistulous communication with the oesophagus. Following further stabilization, the patient underwent repeat procedure with identification of a tear in the lower third of the oesophagus. The patient was subsequently managed as an oesophageal perforation with no fluid or oral intake and was commenced on peripheral total parenteral nutrition prior to definitive primary repair.


CT scan demonstrating patent stent with no suggestion of endoleak and lack of contrast in aneurysm sac.
DISCUSSION
We describe a rare presentation of a probable contained traumatic aortic rupture from a historical high-velocity road traffic accident presenting as an aorto-oesophageal fistula in later life. There are sparse cases in written literature discussing this life-threatening complication. With the advent of trauma guidelines and recent advances in trauma medicine, it is likely that this complication is very unlikely to be described in the future for patients who attend hospital following high-impact trauma due to the high-quality diagnostic imaging that is readily available for this cohort if patients. The triad of dysphagia, occult gastrointestinal blood loss and CT findings of a large aneurysmal aorta should always lead to the diagnosis of an aorto-oesophageal fistula until proven otherwise. Furthermore, extrinsic compression of the oesophagus with any aortic pathology or the presence of locules of gas within the aneurysm sac should be highly suspicious for the presence of an aorto-oesophageal fistula. Onset of symptoms such as dysphagia and a minor bleed (sentinel bleed) should result in prompt referral and discussion with cardiothoracic unit for definitive management. Initial management should focus on resuscitation, stabilization and transfer to unit for definitive management. This case report illustrates the risk and management of ensuing sequelae such as the risk of re-rupture and persistent communication which also would need definitive surgical management.
CONFLICTS OF INTEREST
None to Declare.
FUNDING
Nothing to declare.



