-
PDF
- Split View
-
Views
-
Cite
Cite
Mohamad Moussa, Mohamed Abou Chakra, Baraa Dabboucy, Athanasios G Papatsoris, Youssef Fares, Seizure as the first manifestation of transitional cell carcinoma of the renal pelvis, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa126, https://doi.org/10.1093/jscr/rjaa126
Close - Share Icon Share
Abstract
Upper tract urothelial carcinoma (UTUC) is a rare genitourinary entity of the renal pelvis and the ureter characterized by an aggressive behavior. Cisplatin-based chemotherapy is the first-line therapy of metastatic UTUC. However, a large number of patients with metastatic UTUC are considered ineligible for cisplatin. Immunotherapy emerged as a promising treatment in this setting. Brain metastasis from UTUC is unusual, occurring most often in the presence of systemic metastases. Local therapies such as stereotactic radiosurgery, neurosurgical resection and whole-brain radiotherapy (WBRT) remain the main therapeutic options for brain metastasis. We report a case of a 65-year-old male patient presenting with generalized tonic–clonic seizure. Imaging studies confirmed the presence of multiple brain metastasis. During an evaluation for the primary, he was found to be having metastatic UTUC of the renal pelvis. The brain metastases were treated by hippocampal sparing WBRT with minimal neurotoxicity. The primary tumor was treated by pembrolizumab.
INTRODUCTION
Upper tract urothelial carcinoma (UTUC) is an uncommon cause of tumors worldwide; it accounts for 5% of urothelial cancers. Radical nephroureterectomy is the gold standard treatment for UTUC patients [1]. Among UTUCs, pyelocaliceal tumors are twice as common as ureteral tumors [2]. Lymph nodes, lung, liver, bone and peritoneum are the most common metastatic sites of UTUC [3]. Brain metastases are the most common intracranial tumor. Among adults, the most common origins of brain metastasis (BM) include primary tumors of the lung, breast, skin and gastrointestinal tract. BM from urothelial carcinoma is very rare [4]. We report a case of a 65-year-old man presented to the hospital with seizures. Radiological imaging showed BM from renal pelvis urothelial tumor as confirmed on biopsy. BMs were treated by whole-brain radiotherapy (WBRT) with hippocampal sparing technique. The patient received also pembrolizumab therapy. During a follow-up period of 12 months, the disease was stable.
CASE REPORT
A 65-year-old male, heavy smoker presented to the emergency department with a new-onset seizure. As per family members, he had 3–5 min of generalized tonic–clonic activity. His past medical history was unremarkable. He has also a history of drowsiness for few months. The patient was in postictal phase for 15 min. He was given a loading dose of phenytoin. After that time, the patient was conscious, cooperative and well oriented in time, place and persons. Cranial nerves’ examination was intact. Neuroexam was non-focal. Vital signs were normal. Examination of the heart, chest and abdomen was normal except for left costovertebral angle tenderness. He had no dysuria or frequency or hematuria. There was no history of headache or neurological symptoms or trauma before to the onset of the seizure.
Laboratory examination was normal except for creatinine 2.8 mg/dl (baseline was 1.1 mg/dl). Urine analysis showed 50 RBC WBC per high-power field.
The patient was admitted to the hospital. Brain magnetic resonance imaging (MRI) revealed multiple multifocal hemorrhagic lesions with surrounding edema involving the cerebellum and both cerebral hemispheres, consistent with hemorrhagic metastatic lesions (Figs 1A, B and 2A, B).
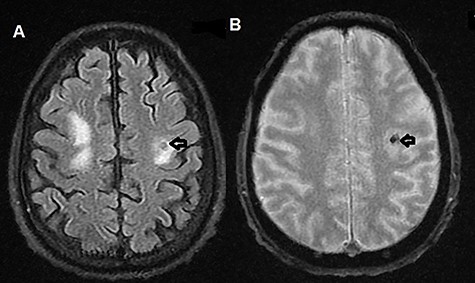
(A) T2-weighted MRI axial image showing left parietal isointense lesion with surrounding edema (black arrow); (B) T2-weighted MRI axial gradient echo sequence showing left parietal lesion compatible with hemorrhagic foci (black arrow).
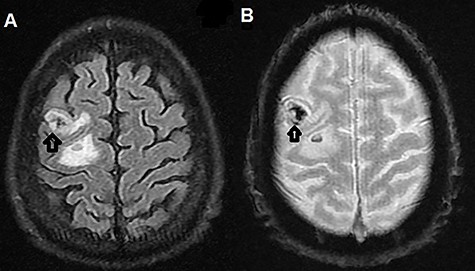
(A) T2-weighted MRI axial image showing right parietal isointense lesion with extensive surrounding edema (black arrow); (B) T2-weighted MRI axial gradient echo sequence showing left parietal lesion compatible with hemorrhagic foci (black arrow).
Computed tomography (CT) scan of the abdomen and pelvis showed poorly marginated soft tissue mass centered at the left renal pelvis (Fig. 3). Multiple prominent and enlarged retroperitoneal lymph nodes are noted. Additional CT chest imaging excluded other metastatic lesions.

Ureteroscopy was done and biopsies were taken from the renal pelvis. Biopsies of the mass showed a high-grade urothelial carcinoma invading the muscularis propria (pT2). Findings were consistent with metastatic UTUC.
This case was discussed at a tumor board meeting. Many members of the tumor board mentioned the potential benefit of WBRT with hippocampal sparing technique as the patient has multiple brain tumors. The discussion focused on the primary treatment for the metastatic UTUC. The patient was considered “unfit” for cisplatin-based combination chemotherapy. Pembrolizumab has been recommended for the patient if testing positive for the programmed death-ligand 1 (PD-L1).
PD-L1–IHC (immunohistochemistry) testing of tumor biopsies was positive (high tumor PD-L1 expression). Pembrolizumab 200 mg IV every 3 weeks was initiated. The irradiated BMs showed continuous regression without relapse in the following 12 months. The clinical and radiologic follow-up with thoraco-abdominopelvic CT for 6 and 12 months showed no disease progression.
DISCUSSION
UTUC accounts for 5% of urothelial carcinomas (UCs), the estimated annual incidence being 1–2 cases/100 000 inhabitants. Systemic chemotherapy is the standard approach for patients with inoperable locally advanced or metastatic UC. Although initial response rates are high, the median survival with combination chemotherapy is about 15 months. In first-line chemotherapy, several cisplatin-based regimens have been proposed [5].
However, up to 50% of patients with unresectable or metastatic UC who had impaired renal function are ineligible for cisplatin-based chemotherapy. Treatment alternatives including carboplatin-based combinations and single-drug chemotherapy are associated with inferior outcomes compared with cisplatin-based chemotherapy. Pembrolizumab and atezolizumab are considered as first-line treatment for cisplatin-ineligible patients with unresectable or metastatic UC [6].
BMs occur in 10–20% of adult patients with cancer and are 10 times more common than primary brain tumors. Therapy for BM includes definitive treatment directed against the tumor itself and supportive treatment. Systemic therapy is not used routinely to treat BM. However, it may be the first therapeutic choice for BM from highly chemotherapy-sensitive primary tumors. Indications for WBRT include the presence of multiple BMs, oligometastases (one to three metastases) with poorly controlled systemic disease, oligometastases too large (>4 cm) for SRS (stereotactic radiosurgery) and reirradiation after late WBRT failure and after surgery or SRS [7].
Outcomes after SRS have been well established, although its exact role in the management of brain metastases is still controversial. Patients with single metastases are a unique population where it seems an ideal situation to implement SRS alone [8]. For patients with a single metastatic lesion in the setting of well-controlled systemic cancer, surgery is highly indicated. Furthermore, surgery remains the only treatment option for patients with life-threatening neurological symptoms, who require immediate tumor debulking [9].
BMs are a very rare presentation of the renal pelvis tumor. There is only one case report of BMs as initial presentation of UC of the renal pelvis in the literature. Kolla et al. reported a case, where patient presented with neurological symptoms. The patient was managed with gamma knife SRS for BMs. The patient had a right renal pelvis UC, for which palliative radical nephroureterectomy was performed, following which he received four cycles of paclitaxel and carboplatin chemotherapy. The patient is alive with stable disease at a 22-month follow-up [10].
In this particular case, we learned that BMs could be an atypical presentation of metastatic renal pelvis UC. We reported this case to alert urologists about the rare manner in which advanced UTUC may sometimes present. Pembrolizumab, being considered a new treatment option for patients who are cisplatin-ineligible candidates for chemotherapy, showed a good clinical response in our case. We also demonstrated that hippocampal avoidance WBRT is a feasible technique and plays an important role to control BMs. This technique better preserves the cognitive function of the patients.
ACKNOWLEDGEMENT
None.
INFORMED CONSENT
Written and signed informed consent was obtained from the patient.
FUNDING
None.
ETHICAL APPROVAL
Our institution does not require ethical approval for case reports.
CONFLICT OF INTEREST STATEMENT
None declared.



