-
PDF
- Split View
-
Views
-
Cite
Cite
Héloïse Tessely, Stéphane Journé, Alexis Therasse, Didier Hossey, Jean Lemaitre, A case of colon necrosis resulting from a delayed traumatic diaphragmatic hernia, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa101, https://doi.org/10.1093/jscr/rjaa101
Close - Share Icon Share
Abstract
We present the case of a 71 years old woman who came at the emergency room for abdominal pain and symptoms of occlusion. The scanner demonstrated a colonic occlusion resulting from an incarceration, diagnosed as a hernia of Bochdalek. But two old rib fractures and a past history of a fall directed us to the diagnostic of delayed diaphragmatic rupture. The patient was operated in emergency and post-operative follow-up was simple. Traumatic diaphragmatic hernias are rarely diagnosed directly after trauma. Complications such as pneumonia, occlusion, enteric ischemia, visceral perforation and twisting of splenic hilium can occur many years after the trauma. This is why, for patients with intestinal obstruction or association of pulmonary abdominal symptoms and history of thoraco-abdominal injury, the diagnostic of diaphragmatic hernia should be considered. When patients present complications, there is a higher rate of morbidity and mortality (31%) reason why, emergency surgery is mandatory.
INTRODUCTION
Post-traumatic diaphragmatic hernia (PTDH) is defined as a displacement of intra-abdominal organs into the chest through a pathological orifice in the diaphragm resulting of a trauma [1].
Diaphragmatic rupture occurs in 5% of severe thoraco-abdominal trauma. The diagnosis is rarely made directly; most of the PTDH are asymptomatic for years until they present complications [2]. Up to 66% of diaphragmatic ruptures are not recognized at the time of trauma [3].
Principals the main etiological mechanisms of PTDH are blunt (80%) or penetrating trauma (20%) [1]. Blunt trauma generates a sudden increase of abdominal and pleural pressure that causes weakness in the diaphragm [2]. Rarely diaphragmatic rupture can occur after surgery, positive pressure non-invasive ventilation or pregnancy [4].
The delay in the diagnosis can be explained because of the negative pressure in the thoracic cavity, which promotes the increase of the initial injury and attracts the visceral organs in the chest [5].
Left diaphragmatic hernias are more frequent (88–95%) than right ones due to a stronger hemi-diaphragm and the protection of the liver which, thanks to its size, prevents the organs to migrate in the thoracic cavity [2].
This is why left-sided PTDH presents with acute symptoms such as obstruction, gastrointestinal symptoms, dyspnoea, chest pain, abdominal pain and vomiting and can evolve to cardiorespiratory failure. Right-sided PTDH have mostly respiratory complaints because of the liver herniation that block the further involving of other viscera [2].
We present in this case report the story of a 71 years old woman with a right PTDH with herniation of the right colic angle presenting as an intestinal occlusion.
CASE DESCRIPTION
A 71 years old woman came at the emergency room for abdominal pain since 7 days and symptoms of occlusion since 4 days. On physical examination, there were signs of peritonitis with a left flank defence.
The biology showed a mild inflammatory syndrome.
An abdominal radiography showed hydro-aeric levels and dilatation of the intestinal bowel (Fig. 1).

The scanner demonstrated a colonic occlusion resulting from an incarceration, which was diagnosed as a hernia of Bochdalek containing the hepatic angle of the colon (Fig. 2–4).

: CT scan images demonstrating a right diaphragmatic hernia containing intestine.
At the relecture of the images, they showed two old rib fractures. When asked to the patient, she mentioned a past history of a fall 2 years earlier, which directed us to the diagnostic of delayed right diaphragmatic rupture.
The patient was operated by anterolateral thoracotomy in the seventh right intercostal space. Reduction of the partially necrotic colon associated with the closure of the diaphragmatic hernia reinforced with a pledged of polypropylene was performed. A chest drain was placed before closure. A laparotomy was also necessary for the segmental colon resection because of signs of advanced ischemia (Figs 5–7).

CT scan images demonstrating a right diaphragmatic hernia containing intestine.
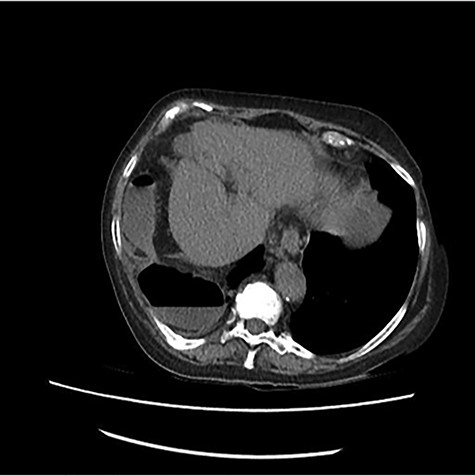
CT scan images demonstrating a right diaphragmatic hernia containing intestine.
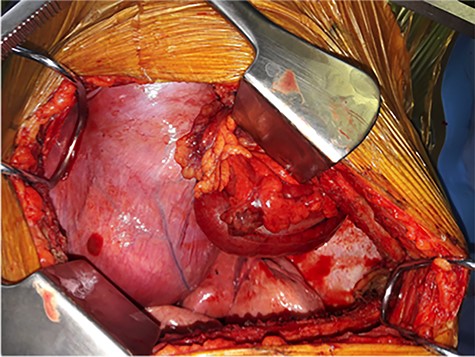
Per-operative pictures, before reduction of the content of the hernia.
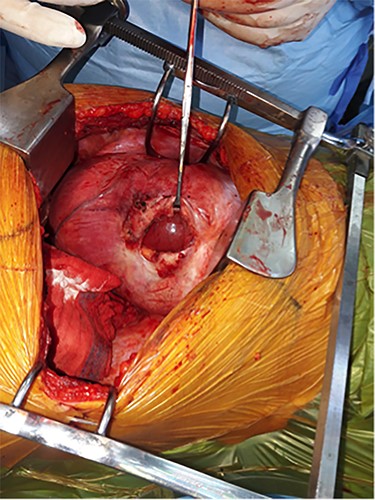
Per-operative pictures, after reduction of the content of the hernia.
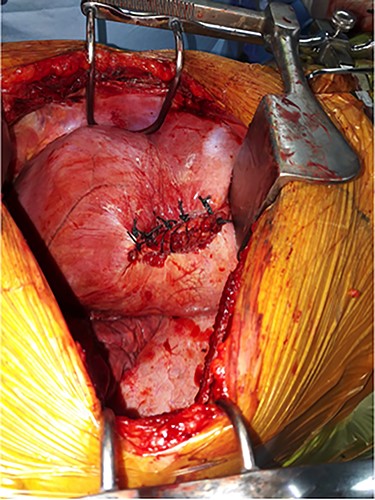
Per-operative pictures, after closure of the diaphragm with pledgets.
At the first post-operative day, 500 cc of blood was found in chest drain. The patient presented tachycardia and hypotension, an emergency thoracoscopy was performed. An active bleeding was found on the inferior pulmonary lobe where there was previously an adherence. Three units of red blood cells and 2 units of fresh frozen plasma were needed.
The next post-operative follow-up was simple and the patient was able to return to her home on the 10th post-operative day.
DISCUSSION
Diaphragmatic lesions were described first by Sennertus in 1541 and the first successful repair was performed by Riofli in 1886 [6].
PTDH can lead to various complications depending of the content of the hernia, such as: pneumonia, intestinal ischemia, perforation, twisting of the stomach or the splenic hilum [5, 7].
Differential diagnosis has to be made with congenital hernias (Boschdalek and Morgagni) that are extremely rare in adulthood.
Chest radiography can already help us to make the diagnosis. The findings that indicate a PTDH can be abdominal contents in the thorax such as a nasogastric tube. An elevated hemi-diaphragm is also suspicious, it is significant when >4 cm higher than the other one. When a distortion of diaphragmatic margin is visible, it has to be investigated. As well as an opacity of the hemi-thorax with mediastinal shift to the contralateral side [2, 6].
Thoraco-abdominal computed tomography (CT) scan is the gold standard for the diagnostic of PTDH with a sensitivity of 71–100% and a specificity of 87% [6]. In addition, CT scan gives us important information such as: the location, the size and the contents of the diaphragmatic hernia [2].
Surgery is always necessary for the treatment of PTDH. When patients present complications and cannot undergo surgery, the mortality rises up to 100% [4].
The surgical reparation can be done by thoracotomy, laparotomy and laparoscopy, with or without mesh.
Association of thoracotomy is necessary in most of the cases of delayed PTDH due to the multiple adhesions between the viscera and the chest. When there are symptoms of obstruction or digestive ischemia, laparotomy is needed [2]. Laparoscopic repairs are more and more done as well for acute and delayed presentation. The advantages are shorter hospital stay, smaller incision, reduced pain and blood loss. Actually, it is recommended for non-complicated presentation of PTDH [8].
Mesh repair is used when the defect is too big to be primarily closed (>25 cm2) [3]. Biological meshes can also be used; it seems that they have many advantages: lower rate of recurrence, better resistance to infections and lower risk of displacement [2]. But there is actually no evidence of the superiority of the utilization of a mesh and the simple raffia is nowadays the most common technique [5].
CONCLUSION
For patients with intestinal obstruction or association of pulmonary abdominal symptoms and history of thoraco-abdominal injury, the diagnostic of diaphragmatic hernia should be considered. When patients present complications, there is a higher rate of morbidity and mortality (31%) reason why, emergency surgery is mandatory.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- ischemia
- abdominal pain
- lung
- emergency service, hospital
- follow-up
- diaphragmatic hernia
- hernia, diaphragmatic, traumatic
- intestinal obstruction
- necrosis
- pneumonia
- rib fractures
- wounds and injuries
- abdomen
- colon
- diagnosis
- morbidity
- mortality
- spleen
- diaphragm, rupture of
- hernia of foramen of bochdalek, congenital
- emergency surgical procedure



