-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel Page, Rasika Hendahewa, An incarcerated Spigelian hernia with the appendix in the sac passing though all layers of the abdominal wall: an unusual cause for chronic right iliac fossa pain, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa099, https://doi.org/10.1093/jscr/rjaa099
Close - Share Icon Share
ABSTRACT
Abdominal wall hernias are a common pathology and source of morbidity including chronic pain. They occur in various anatomical areas; amongst the rarest locations is the Spigelian hernia accounting for <2% of all abdominal hernias. We present a case report of a patient with chronic right iliac fossa pain caused by an incarcerated Spigelian hernia containing her appendix within the hernial defect. Rarer still is that her hernial defect penetrated all three layers of anterior abdominal wall, typically a Spigelian hernia would only pass through transversus abdominis and internal oblique layers.
INTRODUCTION
The presentation of right iliac fossa (RIF) pain both acute and chronic is a common presentation with a wide and varying differential diagnosis. Common differentials include gastrointestinal causes; acute appendicitis, ileitis, colitis and diverticulitis. Ovarian causes; torsion, ruptured cyst, ectopic pregnancy and Mittelschmerz. And a variety of other common causes include mesenteric adenitis, ureteric calculi and more rarely Meckel’s diverticulitis. We present a rare cause of chronic RIF pain in the form of an incarcerated Spigelian hernia containing the appendix.
Spigelian hernias are abdominal wall hernias caused by a defect within transversus abdominis and internal oblique aponeurosis that form the linea semilunaris of the anterior abdominal wall and typically occur below the arcuate line. Usually in this type of hernia the external oblique layer remains intact and a very rare finding is with a defect in all three layers [1–3].
A Spigelian hernia is rare with a reported incidence of 0.12–2% as a cause of all abdominal wall hernias [1–3]. Risk factors for developing a Spigelian hernia are the same as all other abdominal hernias and include chronic increased intra-abdominal pressure from conditions that result in chronic cough, obesity and ascites as well as people with connective tissue disorders such as Ehlers Danlos syndrome and also advancing age and smoking [2].
They are often asymptomatic but can cause significant pain and morbidity the most concerning complication is in the event of bowel herniating through the defect with subsequent strangulation and perforation. Due to their typical anatomical formation with the anterior oblique layer been intact they can be difficult to diagnose clinically particularly in those with a large body habitus. Given its difficulty to diagnose they should be considered as a cause for anyone presenting with unexplained abdominal pain [4, 5].
The investigations of choice for diagnosing and defining Spigelian hernias are dynamic ultrasound and or computed tomography (CT), but keeping in mind defects may not be as obvious in absence of herniation of abdominal contents and therefore lower the sensitivity of any imaging investigation [4, 6]. If these investigations are unremarkable but there is a high clinic suspicion then a diagnostic laparoscopy is an option.
CASE STUDY
A 70-year-old female was referred to the general surgical outpatient clinic with ~18 month history of intermittent dull pain in the RIF that could be exacerbated on movement. She had no associated gastrointestinal symptoms, no associated gynaecological symptoms or systemic features of infection. She had a past medical history of non-alcoholic fatty liver disease, hypertension and Gastro-oesophageal reflux disease (GORD). Surgically she had a previous pfannenstiel incision caesarean section and laparoscopic right oophorectomy and salpingectomy for a concerning ovarian cyst that turned out to be a benign serous cystadenoma. She had been previously investigated with unremarkable ultrasound scans and a normal colonoscopy. Clinically this lady was obese with an overlying lower abdominal pannus with a visible scar from her previous pfannensteil incision in the midline. She was tender in the RIF away from this, no palpable masses or abdominal wall defects were palpable however they would be clinically difficult to appreciate given her body habitus.
A contrast CT scan of her abdomen and pelvis was performed, this demonstrated a right sided Spigelian hernia with a 15 mm neck with the appendix and a small amount of fat within the hernial sac and caecum lying against mouth of the hernia intra-abdominally (Fig. 1 A and B).
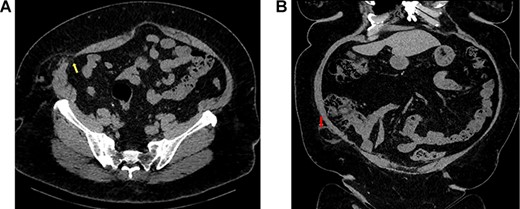
(A) Axial view of CT abdomen and pelvis demonstrating Spigelian hernia with an abdominal wall defect through all three layers of abdominal wall (yellow arrow); (B) coronal view of the same scan demonstrating the appendix herniating through the defect in hernial sac (red arrow).
The optimal management for this patient would be for a repair of the hernia with or without appendicectomy depending on the laparoscopic findings. However the patients preference at the time of diagnosis was to avoid surgery, and she elected for observation and accepted the potential risk of strangulation and perforation of the appendix.
DISCUSSION
Spigelian hernias are a rare type of abdominal wall hernia accounting for 0.12–2% of all abdominal hernias. They share same common risk factors as all abdominal wall hernias as discussed above. Often, they can be asymptomatic but can cause pain or discomfort when abdominal contents herniate through the defect with the worst case scenario been strangulation of bowel with subsequent ischaemia and perforation.
Optimal management of these hernias is via surgical repair of which several techniques are described. Historically, the mainstay of repair has been with an open transverse incision with primary suture repair with or without mesh. However, the preferable option today is a laparoscopic repair and is of great utility in patients with obesity where it may be difficult to clinically isolate the exact location of the hernia [3]. The laparoscopic technique involves entering the peritoneum with laparoscopic ports, creating a peritoneal flap and reduction of sac and contents followed by a variety of methods that involve primary closure via laparoscopic suturing with mesh reinforcement or by repair with mesh alone [3, 7].
In summary Spigelian hernias are rare, can be difficult to diagnose and have a high rate of strangulation of contents between 17 and 24% [3]. Given these factors the clinician should have a high degree of clinical suspicion particularly in patients presenting with chronic lower quadrant pains that cannot be attributed to another cause. Our patient chose for conservative management at the time of diagnosis accepting the risk factors associated with not having a repair of the hernia.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



