-
PDF
- Split View
-
Views
-
Cite
Cite
William G Aguayo, Christian L Rojas, Gabriel A Molina, Javier Cisneros, Hernan V Reyes, Hugo Efrain Haro, Incidental finding after laparoscopic gastric sleeve, the value of pathology, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa121, https://doi.org/10.1093/jscr/rjaa121
Close - Share Icon Share
Abstract
Gastric neuroendocrine tumors (NET) are rare tumors with a broad spectrum of symptoms; in recent years, the number of cases has increased due to the growing number of upper endoscopies. Obesity has become a worldwide epidemic and bariatric surgery one of the most effective therapies to control this illness. As more surgeries are performed, the number of histopathological samples will also increase. Incidental discoveries on these histopathological specimens are difficult situations to encounter as medical plans, prognosis and therapy will have to change accordingly. We present the case of a 43-year-old patient who underwent a laparoscopic gastric sleeve. On pathology, a NET was detected, and additional surgery was required. On follow-ups, the patient is doing well.
INTRODUCTION
Obesity has become a worldwide health problem and ordinary diets and exercise regimes have failed to control this illness [1, 2]. Bariatric surgery has become the treatment of choice and laparoscopic gastric sleeve (LGS) is one of its most effective surgeries to control it [3]. Usually, histopathological specimens retrieved after surgery are normal, nonetheless, on rare occasions, pathology findings will make us change our entire therapeutic plan [1, 4]. We present a case of a 43-year-old patient with obesity. An incidental neuroendocrine tumors (NET) was found after an LGS; thus another surgery was required and the patient underwent full recovery.
CASE REPORT
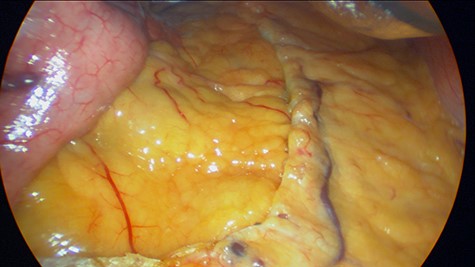
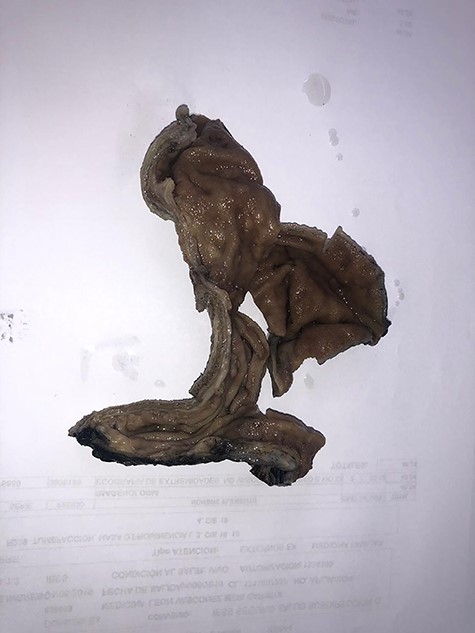
Patient is a 43-year-old female with past medical history of hypothyroidism and obesity. She sought surgical consultation since her body mass index (BMI) was high (36) and she had failed numerous attempts to lose weight over the past 10 years. Preoperative exams including an upper endoscopy were normal. LGS was planned. During the procedure, we used one 15 mm port, one 12 mm port and three 5 mm ports. A 30 telescope was used during the procedure to achieve visualization of the angle of his, a grasper was used as a liver retractor and a 36 French bougie was inserted to decompress the stomach. The incisura was located and a small window in the lesser sac was created 4 cm away from the incisura, the omentum was mobilized cranially, the bougie was advanced to the first part of the duodenum and staplers were used to create the sleeve. (Fig. 1) After this, the staple line was reinforced using a 3-0 synthetic absorbable monofilament suture (PDS 3-0, Ethicon, Johnson & Johnson). The specimen was retrieved from the 15 mm port, and the procedure was completed without complications. During the procedure, no lymph nodes or masses were seen. The patient underwent full recovery and was discharged without any apparent complications. Five days later, pathology reported that on the specimen, a small 4-mm polyp was detected in the staple line in the upper part of the fundus, a finding that was not detected on the previous endoscopy. After further evaluation, a grade II well-differentiated multifocal neuroendocrine tumor with vascular and perineural invasion was detected. Ki 67 index was 17% and 3/10 hpf mitosis were discovered (Figs 2, 3A and B).
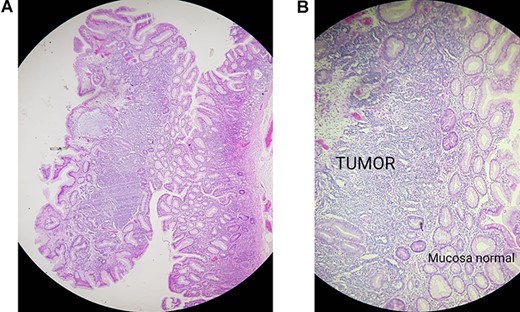
(A) Pathology, gastric mucosa, (B) pathology, tumor invading the gastric muscle.
The prognosis changed immediately, the patient was immediately notified of this finding and a new contrast-enhanced computed tomography revealed no masses or lymph nodes, therefore a D2 radical gastrectomy reconstructed with an esophagojejunal roux-en-y was performed, a drain was placed near esophagojejunal anastomosis and the remainder of the procedure was achieved without any complications. Pathology reported the same neuroendocrine tumor without lymph nodes involvement. After recovery, oncologist consultation was needed and five cycles of adjuvant chemoradiotherapy were achieved. One year after initial surgery and after psychiatric aid, the patient is doing well.
DISCUSSION
NET or carcinoid tumors are rare neoplasms first described by Lubarsch in 1888 [1, 11]. These tumors are spread throughout the body but are mainly found within the gastrointestinal tract. Gastric NET arise from the enterochromaffin-like cells and represent 7–8% of all NETs and about 0.1–0.6% of all gastric cancers [1, 3]. Although uncommon their incidence is increasing due to the widespread use of upper digestive endoscopy [1, 4]. Obesity has been increasing both in developing and developed countries becoming an epidemic [2, 5]. Over one billion people in the world are overweight with a BMI between 25 and 30 kg/m2, and 300 million people are obese (BMI > 30 kg/m2) [2, 3]. Obesity causes severe health problems, like diabetes, cancer, hypertension and hyperlipidemia [2].
Bariatric surgery has become the most effective way to lose weight, reduce comorbidities, improve quality of life and diminish all-cause mortality [2, 3]. Roux-en-Y gastric bypass, LGS and gastric banding are the most common surgical bariatric procedures [2, 6]. Of these, LGS is the only surgical procedure that provides a specimen for histopathological examination [2, 3]. Before any procedure, bariatric patients often endure thorough preoperative and nutritional evaluation [2, 7]. Preoperative upper endoscopy is generally not advised by the American Society for Metabolic and Bariatric Surgery, while other guidelines suggest its use, as many conditions including esophageal webs, duodenal ulcers or masses can be detected (5% of the cases) [2, 3, 8]. In our case, preoperative endoscopy was performed although it did not identify the tumor.
After LGS, unanticipated histopathological findings are found in almost 65% of the cases, of these patients, up to 8.4% will need additional follow-up [3]. Helicobacter pylori, autoimmune gastritis, intestinal metaplasia, chronic gastritis, tumors (Gastric Glomus, GIST, etc.), among others have been detected [2, 6, 9]. In our case, a NET was discovered.
Recent observations have shown a higher incidence of carcinoid tumors in obese patients, nonetheless further studies are needed [7, 8]. Treatment of gastric carcinoids is based upon its classification and clinical stage. Complete excision of the lesion either endoscopically or surgically must be done to improve the patients’ outcomes [1, 10]. In our case, as the tumor was found in the staple line, additional surgery was required.
Surgeons must be conscious of the high prevalence of unanticipated histopathological in bariatric patients, close monitoring and evaluation of pathology reports from any specimen are obligatory as its findings may impact our management and the patients’ prognosis.
Surgery and pathology are invaluable allies, the quality of our care will depend on our teamwork and our commitment to patients.
Funding
No funding.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
REFERENCES



