-
PDF
- Split View
-
Views
-
Cite
Cite
Jeffrey M Breton, Michael J Yang, Ron I Riesenburger, The use of decompressive segmental sublaminoplasty to treat myelopathy caused by lumbar stenosis in tethered cord syndrome, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa041, https://doi.org/10.1093/jscr/rjaa041
Close - Share Icon Share
Abstract
A 79-year-old woman presented with acute-onset right leg pain in the setting of 3 months of progressive gait deterioration and bilateral leg weakness. On exam she had right lower extremity hyperreflexia and weakness. Lumbar spine magnetic resonance imaging demonstrated L3–L5 central canal stenosis with L4–L5 spondylolisthesis and a previously undiagnosed tethered cord. She underwent minimally invasive left segmental sublaminoplasty at L3–L4 and L4–L5 for spinal cord decompression with onlay arthrodesis resulting in resolution of her radicular pain and improved strength. This is a unique case of lumbar spinal stenosis presenting with myelopathy in the context of a previously asymptomatic and undiagnosed tethered cord.
INTRODUCTION
Tethered cord syndrome (TCS) is an uncommon clinical and radiologic syndrome in which patients typically present with progressive back pain, lower extremity weakness and bladder dysfunction with findings of a low-lying conus medullaris at or below the L2 vertebral body and a thickened filum terminale on magnetic resonance imaging (MRI). It is rare in adults and is most common postmyelomeningocele (MM) repair or associated with an intradural lipoma. Lumbar spinal stenosis often results from degenerative spondylotic changes including hypertrophied ligamentum flavum and/or facet joints and classically presents with neurogenic claudication. Here we present a unique case of lumbar spinal stenosis in a patient with TCS that resulted in lumbar myelopathy.
CASE DESCRIPTION
A 79-year-old female with insulin-dependent diabetes mellitus presented with acute-onset right leg pain without preceding trauma, in the context of 3 months of gait deterioration. Over that time, she had progressed from ambulating independently to requiring a walker. She had no history of spinal dysraphism, myelopathy, spinal surgery or previous neurologic deficit, only noting chronic intermittent lower back pain. Her leg pain had been managed conservatively with a course of steroids and gabapentin that effectively relieved the pain, though she continued to have residual right leg weakness.
On exam, she exhibited weakness in her right iliopsoas, quadriceps, anterior tibialis and extensor hallucis longus muscle groups with pathologic hyperreflexia and markedly increased right lower extremity tone. Noncontrast lumbar spine MRI revealed L4–L5 anterolisthesis and a previously undiagnosed tethered cord with her conus medullaris extending to the L5–S1 level (Fig. 1), in addition to L3–L4 and L4–L5 central canal stenosis (Fig. 2A and B).

Preoperative T2 sagittal MRI demonstrating a tethered spinal cord continuing caudal to compression at L3–L4 and L4–L5 with the conus medullaris extending to L5–S1.
She subsequently underwent uncomplicated left L3–L4 and L4–L5 segmental sublaminoplasties for effective central canal decompression. An onlay arthrodesis was completed at those levels to promote joint fusion after decompression in the setting of L4–L5 anterolisthesis. Postoperatively, the patient had slightly improved right leg strength and was discharged to a rehabilitation facility on postoperative day one. Six weeks postoperatively, she reported near complete resolution of the radicular right leg pain and improving right leg strength.
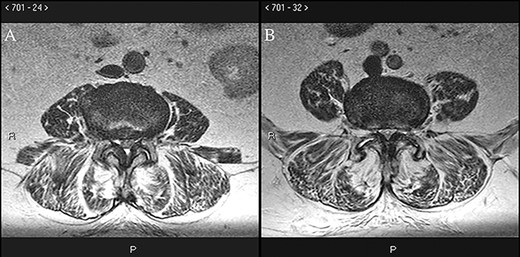
Preoperative axial T2 MRI at the L3–L4 (A) and L4–L5 (B) levels demonstrates ligamentous hypertrophy and central canal stenosis with cord compression.
DISCUSSION
Myelopathy, including pathologic hyperreflexia, is a unique presentation for lumbar spinal stenosis, which classically presents with neurogenic claudication, a phenomenon of lower extremity pain, weakness and numbness that is worsened with spinal extension and is not relieved at rest [1]. TCS is a clinical and radiologic syndrome most often presenting with lower extremity pain, sensory and/or motor deficits, and bladder or bowel dysfunction in the setting of a conus medullaris lying caudal to the L2 vertebral body and a filum terminale greater than 2 mm thick. It is more common in children, and adult-onset is classically associated with precipitating events such as stretching of the conus medullaris, narrowing of the spinal canal, or trauma [2]. Lumbar spinal stenosis presenting with myelopathy in the setting of TCS has been previously documented as a rare complication in adults who underwent myelomeningocele (MM) repair as children and later developed a tethered cord [3]. The vast majority of patients with MM repairs have radiographic evidence of a tethered cord later in life, though only 10–30% develop TCS [4]. MM repair is associated with 4–14% of TCS cases, with other causes including intradural lipomas, split cord malformations, meningoceles, diastematomyelia and thickened or fatty filum terminale [5]. The case presented here is unusual, as the patient had no history of spinal surgery or dysraphism and her tethered cord was identified at the age 79 years, compared to the average age of adult-onset tethered cord of 33–46 years old [2, 6].
Previous studies do not demonstrate a clear benefit to treating asymptomatic tethered cord, though earlier intervention when symptoms do develop improves outcomes [6]. Surgical detethering has been shown to improve TCS symptoms, particularly back and leg pain, in the majority of cases, and patients presenting with motor weakness tend to improve after surgery more than those with sensory loss or urinary symptoms [7]. TCS has been treated with open and minimally invasive techniques for detethering, including mini-open and pedicle subtraction osteotomy [8, 9]. Retethering has been reported following 25–80% of untethering surgeries for TCS in post-MM repair patients, whereas less than 10% of patients with TCS and history of closed dysraphism experience retethering [5].
In this case, bilateral L3–L4 and L4–L5 decompression via unilateral hemilaminectomies (also known as segmental sublaminoplasty) without cord detethering was an effective minimally invasive technique for treating the patient’s weakness and myelopathy. She was not a good candidate for instrumented fusion for spondylolisthesis due to her advanced age, diabetes mellitus and increased risk of spinal cord injury. In conclusion, this unique case demonstrates decompressive segmental sublaminoplasty as an effective treatment for multilevel lumbar spinal stenosis causing myelopathy in a patient with a previously undiagnosed tethered spinal cord, with short-term follow-up revealing improvement in her right leg pain, weakness and myelopathic symptoms.
Conflicts of interest statement
The authors report no conflicts of interest.
References
- magnetic resonance imaging
- surgical procedures, minimally invasive
- asthenia
- bone marrow diseases
- constriction, pathologic
- spinal cord diseases
- leg
- lumbar spinal stenosis
- lower limb pain
- tethered cord syndrome
- hyperreflexia
- lower extremity paresis
- spinal cord central canal
- undiagnosed
- third lumbar vertebra



