-
PDF
- Split View
-
Views
-
Cite
Cite
André C Pacheco, Maria J Jervis, Joana Pimenta, Ricardo Escrevente, Fátima Caratão, Internal double omental hernia: a rare cause of acute abdomen, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa038, https://doi.org/10.1093/jscr/rjaa038
Close - Share Icon Share
Abstract
Small bowel obstruction is one of the most common causes for acute abdominal pain leading to surgical admissions, occurring most frequently due to postoperative adhesions. Although less common, internal hernia is also a possible etiology, in which a delay on its therapy may lead to a not so dismal morbidity and mortality. Here, we report the case of a 24 year old Caucasian man that was admitted in our emergency department with an inaugural episode of sudden-onset epigastric pain associated with vomiting. After observation and diagnostic workup, the patient underwent urgent laparotomy that revealed an ischemic small bowel due to a double omental hernia, being successfully treated without enteric resection.
INTRODUCTION
Internal hernia is an uncommon cause of small bowel obstruction, with an overall incidence of less than 1% and usually asymptomatic [1].
Transomental hernia, which is seldom diagnosed preoperatively, comprises about 1–4% [2] of all internal hernias. A double omental hernia denotes herniation of the small bowel through an opening in the gastrocolic omentum and exits through the gastrohepatic omentum, representing an extremely rare cause for small bowel obstruction.
Due to its unspecific clinical symptoms and possible accelerated progression of disease, one should keep a high grade of suspicion and a low threshold for surgical intervention.
CASE REPORT
This is a case of a 24 year old Caucasian sportsman with a smoking habit (5 pack-years), who was admitted in our emergency department with an inaugural episode of sudden-onset epigastric pain associated with nausea and vomiting, in the previous 6 hours. Questioned about trauma, chest pain, respiratory disorders or other gastrointestinal complaints, he denied all symptoms.
The abdomen had a tympanic percussion in the upper quadrants and tenderness in the epigastric area. He also presented with tachycardia, without other relevant findings. The laboratory studies revealed increased white blood cell count (WBC) and air-fluid levels on the abdominal x-ray (Fig. 1). Due to high suspicion of small bowel obstruction, an abdominal computed tomography was performed, revealing signs of an internal hernia of unknown type (Fig. 2).
An exploratory laparotomy was then performed, which revealed herniation of jejunal loops through the gastrocolic ligament to the lesser sac, then protruding through a defect in the gastro-hepatic ligament (Figs 3 and 4). The initial ischemia of the bowel reverted after reduction and the omental defects were corrected. Of note was the frailty of the great omentum due to its very low adipose content.

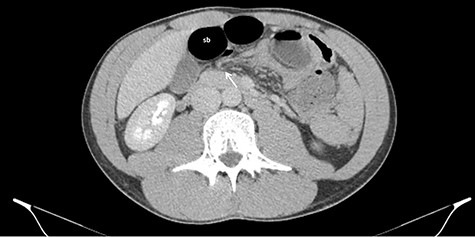
Axial CT images of dilated small bowel (sb) with the respective mesentery converging to the hernia defect (white arrow) in the gastrohepatic ligament.

Sagittal CT images with small bowel protruding the gastrocolic omentum (white arrow) to the lesser sac, pushing the stomach (s) upward.
The patient was discharged on the fourth postoperative day, with no complications during follow-up appointments.
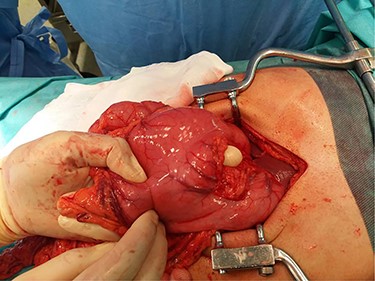
Cephalocaudal orientation from right to left. Hand inserted through the gastrocolic ligament defect and second finger protruding from the gastrohepatic defect.
DISCUSSION
Transomental hernia is a rare entity, representing 1–4% of all internal hernias [2, 3]. An internal hernia is defined as a protrusion of viscera across an intraperitoneal opening in the abdominal cavity. Double omental hernias have also been reported and are extremely rare [3, 4].
The hernial orifices may be congenital or acquired. Anomalies of peritoneal attachment and intestinal malrotation may result in congenital hernias, occurring most frequently in the paraduodenal fossae. Other causes of internal herniation are inflammation, trauma and as complications from previous surgeries [5, 6].
Transomental hernias are frequently caused by complications of previous surgery, nonetheless, altered anatomy of the liver, lesser sac, mesentery or presence of adhesions have been reported as predisposing factors for transomental hernias [3]. A spontaneous transomental hernia may be explained by the atrophy of the greater omentum in patients without the predisposing factors mentioned above [7].
The diagnosis of a transomental hernia is difficult to attain, due to its clinical heterogeneity, varying from mild, intermittent abdominal pain to acute severe pain accompanied by nausea and vomiting, as it was in the present case. Its diagnosis is usually made during emergent laparotomy for acute intestinal obstruction.
Abdominal computed tomography is the gold standard for the diagnosis, usually showing incarceration of a dilated intestinal loop. Although it might be difficult to differentiate the type of internal hernia causing the obstruction, characteristic features of transomental hernias have been described as dilated bowel loops without a sac-like appearance located in the most anterior portion of the peritoneal cavity with omental vessel running vertically around the hernia orifice [5].
Transomental hernia is more frequently associated with presentation with gangrenous bowel, in comparison to other internal hernias [6]; therefore a rapid diagnosis and treatment are essential. Although rare, internal hernias are a potentially life-threatening condition when acute intestinal obstruction occurs, with mortality rates exceeding 50% [5].
The operative management includes reduction of the hernia content, resection of ischemic, necrotic or perforated viscera and repair of the hernia orifice. Mild ischemia of the incarcerated bowel may be reversed several minutes after reduction, as occurred in the presented case.



