-
PDF
- Split View
-
Views
-
Cite
Cite
David Fan, Stephanie Luster, Ibrahim G Eid, Abdul Saied Calvino, A multidisciplinary approach to carotid body tumors surgical management, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa030, https://doi.org/10.1093/jscr/rjaa030
Close - Share Icon Share
Abstract
Carotid body tumors (CBTs) are rare and usually require complex surgical resection. We present a case of a large 7-cm CBT successfully treated in a community cancer center using a multidisciplinary team approach.
A 32-year-old male referred for surgical evaluation of an asymptomatic right neck mass. CT angiography showed a 7-cm tumor encasing the carotid vessels, including the bifurcation (Shamblin III). Preoperative angiography and embolization were performed by interventional radiology. The patient underwent surgical removal of the CBTs and required surgical reconstruction with a common carotid to internal carotid bypass using a polytetrafluoroethylene interposition graft. The hypoglossal nerve, vagus nerve and glossopharyngeal nerve were identified, meticulously dissected and preserved. The patient did well after surgery and recovered with no complications. This report examines the diagnosis, preoperative workup and surgical management of CBTs using a multidisciplinary team approach.
INTRODUCTION
Derived from neuroectodermal tissue, carotid body tumors (CBTs) are the most common type of paraganglioma in the head and neck region. CBTs can be sporadic in 5–10% of the cases and familial in up to 30% [1]. The majority of these tumors are found incidentally during inspection and palpation of the neck for unilateral swelling. If symptoms are present the most common are pain, dysphagia and autonomic dysfunction. If left untreated, malignant potential and local invasion can lead to life-threatening complications.
First described by von Haller in 1743, the carotid body is a reddish-brown, well circumscribed, highly specialized round organ, 2–6 mm in size, located in the adventitia of the carotid bifurcation [2]. Blood supply comes primarily from the ascending pharyngeal branch of the external carotid artery (ECA) and innervation through the glossopharyngeal and vagus nerves. Differential diagnosis includes cervical lymphadenopathies, lateral cervical cysts, branchial cysts, vagal paragangliomas, thyroid nodules, carotid artery aneurysms and parotid gland tumors. Complete surgical excision is the treatment of choice [3]. In this case report, we describe the preoperative work up, surgical technique and the clinical outcome of a patient with a large CBT.
CASE REPORT
A 32-year-old male referred for surgical evaluation of an asymptomatic, 7 cm, right neck mass. There was no family history of paragangliomas or evidence of multiple paragangliomas. Initial work up included a bilateral neck ultrasound that showed a hypervascular, hypoechoic mass on the right carotid artery bifurcation. Then, a computed tomography angiography (CTA) was done and showed the tumor encasing the carotid vessels, including the bifurcation consistent with a Shamblin III CBT (Fig. 1). Biochemical testing with 24-h urine catecholamines was negative.

(A) CTA sagittal view, white arrow pointing to the CBTs encasing the ICA and ECA corresponding to Shamblin III. (B) CTA coronal view, white arrow pointing at the CBTs.
Preoperative Preparation
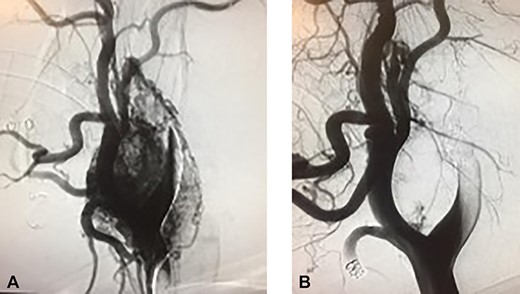
The CBT was nonfunctional and therefore no preoperative alpha blockade was needed. The patient underwent preoperative angiography and embolization by the interventional radiology team to decrease the risk of intraoperative bleeding given the size (7 cm) and the Shamblin III classification (Fig. 2A and B). The surgery was performed a week later by the surgical oncology team assisted by a vascular surgeon.
The Operation
Incision was made from the angle of the mandible towards the chin and subplatysmal flaps were created. The common carotid artery was dissected to obtain proximal control. Distal control was obtained by exposing the internal carotid artery and the ECA cephalad to the tumor (Fig. 3). The tumor was adherent to the posterior wall of the carotid bifurcation, requiring en-bloc resection (Fig. 4) with reconstruction using a common carotid to internal carotid bypass performed with a 6-mm polytetrafluoroethylene (PTFE) interposition graft (Fig. 5). The hypoglossal, vagus and glossopharyngeal nerves were identified, meticulously dissected and preserved. The patient recovered well, had hoarseness of the voice, which resolved after few months with no intervention. The tumor pathology revealed an extra-adrenal paraganglioma positive for chromogranin, synaptophysin and S-100.
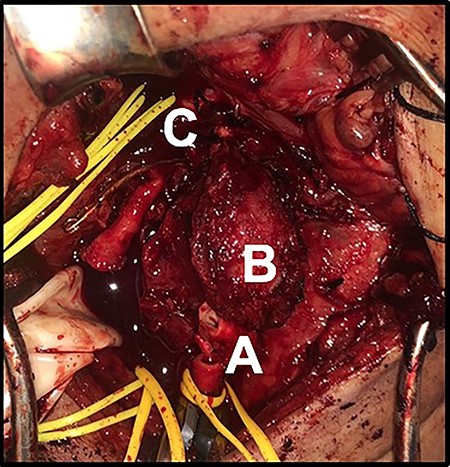
(A) Tumor at the bifurcation. Transected common carotid artery. (B) CBTs. (C) Internal carotid artery.

CBTs specimen, posterior view with the bifurcation attached to it.

DISCUSSION
Classification of CBTs based on the relationship with the carotid vessels, such as the Shamblin classification, has been used to assess resectability and associated surgical morbidity. Shamblin et al. [4] classified the tumors in three types, type I tumors are localized masses and do not involve in more than 180° the surrounding carotid arteries. Type II tumors involve more than 180° the carotid arteries. Type III tumors are large and encase the carotid vessels. Type III tumors are the most difficult type to resect and are associated with higher rate of neurovascular complications [4]. One of the limitations of the Shamblin classification is the inability to predict safely dissection of the carotid vessel’s and the need of vascular reconstruction. The use of MRI to predict the need of vascular reconstruction has been evaluated, showing correlation between the degree of circumferential contact of the ICA with the tumor and the need of reconstruction [5]. Like seen in our case, most of Shamblin III tumors have involvement of the adventitia and usually require vascular reconstruction. A classification system that combines Shamblin criteria with degree of vessel involvement by MRI might be more accurate way to predict the need of vascular reconstruction.
Preoperative embolization of CBTs remains a controversial topic. The risks include postembolization morbidity such as transient ischemic attack and even stroke by embolic particles [6].
The inflammatory effects of preoperative embolization could make precise subadventitial dissection more difficult. Benefits of preoperative embolization include decrease of tumor size facilitating complete resection and decreased blood loss. Currently, embolization seems to be beneficial for tumors larger than 5 cm, Shamblin’s type III, and those with significant cranial extension [7]. Correlation between preoperative embolization and vascular reconstruction has not been established.
An estimated of 35% of patients with CBTs have hereditary predisposition. The succinate dehydrogenase (SDH) subunit D (SDHD) has been recently located in paraganglioma gene locus 1 (PGL-1) [8], the SDHD mutation has been found in 52% of those with germline mutations in the SDH gene locus. Younger age at diagnosis, symptomatic presentation, positive family history and multiple paragangliomas have been associated with SDH gene mutation [9]. Our case presented at a young age but with no symptoms, no family history and no evidence of multiple paragangliomas and therefore genetic testing was not performed. The mean age of patients presenting with familial predisposition to CBTs has been reported between 30 and 36 [10], these patients should be evaluated if other factors are present such as multiple paragangliomas or family members with the disease. In those cases, SDH mutation analysis should be offered. Identification of this mutation can help in planning long-term surveillance and identification of family members that could also be at risk of paragangliomas formation.
In conclusion, CBTs resection is a relatively rare procedure. The use of preoperative embolization could be useful to decrease blood loss during surgery. Tumors greater than 5 cm, Shamblin II or III seems to benefit the most from preoperative embolization, but its use should be evaluated in a case-by-case base. Interposition graft for CCA to ICA bypass is necessary when complete dissection of the CBTs from the ICA or CCA is not possible. A multidisciplinary approach for these rare tumors allows for proper preoperative evaluation, surgical planning and a safe resection as seen in our case.
CONFLICT OF INTEREST
None to be disclosed.
Reference
- angiogram
- embolization
- carotid body paraganglioma
- cognitive-behavioral therapy
- glossopharyngeal nerve
- paraganglioma
- patient care team
- polytetrafluoroethylene
- preoperative care
- interventional radiology
- reconstructive surgical procedures
- surgical procedures, operative
- vagus nerve
- diagnosis
- neoplasms
- neck mass
- bypass
- computed tomographic angiography
- excision
- interdisciplinary treatment approach
- interposition graft



